
Classification: Protected A
Guide to Alberta’s
Mental Health Act
Revised Edition October 7, 2022
Classification: Protected A 2
Guide to Alberta’s Mental Health Act
Disclaimer
Material appearing in the Guide to Alberta’s Mental Health Act (guide) may be
reproduced or copied in full for education and program development purposes or not-
for-profit, non-commercial activities without permission.
This document is intended as a guide and as general information only and is not to
replace the advice of legal counsel.
Obtaining Copies
The guide will be available online at the Alberta Health Services (AHS) website:
https://www.albertahealthservices.ca/info/Page3531.aspx
Guide Updates
Please refer to the website above for any changes and/or revisions of a significant
nature to the Guide to Alberta’s Mental Health Act.
This is a revised edition of the guide. Its purpose is to explain the requirements of the
Mental Health Act in plain, easy‐to‐understand language. The guide will be updated as
provisions of the Mental Health Act are brought into force or as the Mental Health Act is
amended.
Guide to Alberta’s Mental Health Act – 2022 Ed.
© 2022 Alberta Health Services
Additional Sources of Information
Mental Health Act and regulations
The Act and regulations can be viewed online or purchased from:
King’s Printer
Main Floor, Park Plaza
10611 – 98 Avenue
Edmonton, AB T5K 2P7
Phone: (780) 427-4952
Website: https://www.alberta.ca/alberta-kings-printer.aspx
Mental Health Act forms
Electronic versions of all the Mental Health Act forms are available on the Alberta
Health Services website at: https://www.albertahealthservices.ca/info/page1256.aspx
These forms can be A) completed on the computer and then printed and signed, or B)
printed then completed by hand and signed. They may not be altered in any way.
Classification: Protected A 3
Contents
The Alberta Mental Health Act - Introduction ................................................................... 8
History of Mental Health Legislation in Alberta ................................................................ 8
Definition of Mental Disorder ........................................................................................... 9
Qualified Health Professional ........................................................................................ 10
Secure Location ............................................................................................................ 10
Cancellation Certificate ................................................................................................. 10
Virtual Health ................................................................................................................. 11
Revised Criteria for Admission Certificates and Renewal Certificates........................... 11
Reasonable Grounds .................................................................................................... 11
Revised Responsibilities of Facility Leadership ............................................................. 11
New Reporting Requirement ......................................................................................... 13
Community Treatment Orders (CTOs) .......................................................................... 13
Mental Health Review Panels (review panels) .............................................................. 14
Mental Health Patient Advocate (Patient Advocate) ...................................................... 14
Protection of Individual Rights within the Mental Health Act .......................................... 15
The Meaning of “the board” in the Act ........................................................................... 16
CHAPTER 1: Designated Facilities ............................................................................... 17
1.1 Introduction to Facilities ...................................................................................... 17
1.2 Voluntary Patients in Designated Facilities ......................................................... 18
1.3 Formal Patients in Designated Facilities ............................................................. 18
1.4 Minors in Designated Facilities ........................................................................... 18
1.5 Forensic Patients in Designated Facilities .......................................................... 19
1.6 Managing Complaints arising within a Designated Facility ................................. 19
1.7 Responsibilities of the Board / Facility Leadership ............................................. 19
CHAPTER 2: Apprehension and Conveyance to a Designated Facility; Detention in a
Designated Facility................................................................................... 25
2.1 Apprehension, Conveyance and Detention ........................................................ 25
2.2 Apprehension and Conveyance by First Admission Certificate (Form 1 -
Admission Certificate) ......................................................................................... 26
2.3 Warrant for Apprehension Issued by a Provincial Court Judge (Forms 7 & 8) ... 28
2.4 Extension of the Warrant (Form 9 - Extension of Warrant) ................................. 29
2.5 Apprehension by a Peace Officer (Form 10 - Statement of Peace Officer on
Apprehension) .................................................................................................... 30
2.6 Apprehension and Conveyance of a Person not Complying with a Community
Treatment Order (CTO). ..................................................................................... 31
2.7 Examination at a designated facility ................................................................... 32
Classification: Protected A 4
2.8 Questions about Apprehension, Conveyance and Detention in Practice ............ 33
CHAPTER 3: Admission and Detention ........................................................................ 35
3.1 Second Admission Certificate ............................................................................. 35
3.2 Contents of Admission Certificates ..................................................................... 36
3.3 How and Why Treatment Plans are Developed? ................................................ 37
3.4 Extending the Detention Period by Renewal Certificates ................................... 37
3.5 Completion of Forms .......................................................................................... 38
3.6 Admission and Detention Arising from an Arrest for Criminal Charges .............. 38
3.7 Application to Cancel Certification and Detention ............................................... 39
3.8 Leave of Absence ............................................................................................... 40
3.9 Transfers ............................................................................................................ 41
3.10 Discharge ........................................................................................................... 42
3.11 Questions about Admission and Detention in Practice ....................................... 43
3.12 Flowchart: Formal Patient ................................................................................... 48
CHAPTER 4: Rights of Formal and Voluntary Patients ................................................. 50
4.1 Notification of Certification and Right to Hearing before Review Panel .............. 51
4.2 Notification of the Right to Communication, Visitors, Legal Counsel, and the
Mental Health Patient Advocate ......................................................................... 52
4.3 Right to Treatment and a Treatment Plan .......................................................... 52
4.4 Right to Consent to or Refuse Treatment ........................................................... 53
4.5 Control ................................................................................................................ 53
4.6 Right of Formal Patients to a Second Opinion Regarding Competency to Make
Treatment Decisions ........................................................................................... 54
4.7 Right of Formal Patients to Apply to Review Panels ........................................... 54
4.8 Right to Appeal to Court of King’s Bench ........................................................... 55
4.9 Questions about Rights of Formal and Voluntary Patients in Practice ................ 55
CHAPTER 5: Mental Health Review Panels ................................................................. 58
5.1 Purposes and Composition................................................................................. 58
5.2 Types of Applications Heard by a Review Panel ................................................ 58
5.3 Conduct of Hearings ........................................................................................... 61
5.4 Refusal to Hold a Hearing................................................................................... 62
5.5 Further Function of Review Panels – Deemed Application for a Hearing ........... 62
5.6 Appeal of Review Panel’s Decisions .................................................................. 63
5.7 The Formal Patient who has a Guardian under the Adult Guardianship and
Trusteeship Act (AGTA) ..................................................................................... 63
5.8 Questions about Review Panels and Hearings in Practice ................................. 65
CHAPTER 6: Competence, Consent and Treatment Decisions .................................... 70
Classification: Protected A 5
6.1 Competence ....................................................................................................... 71
6.2 Minors and Mature Minors .................................................................................. 72
6.3 Consent .............................................................................................................. 73
6.4 Certificate of Incompetence to Make Treatment Decisions................................. 73
6.5 Treatment Decisions Made by a Substitute Decision-Maker .............................. 74
6.6 Challenging the Certificate of Incompetence by Applying to a Review Panel ..... 76
6.7 Second Opinion Regarding Competency when the Formal Patient Objects to
Treatment ........................................................................................................... 76
6.8 Reasons to Apply to a Review Panel for a Treatment Order .............................. 77
6.9 Best Interests Considerations in Treatment Orders ............................................ 78
6.10 Second Opinion of Treatment – Best Interests ................................................... 78
6.11 Psychosurgery .................................................................................................... 79
6.12 Questions about Consent, Competency and Treatment Decisions in Practice ... 79
6.13 Flowchart: Competency & Consent – Formal Patient ............................................ 83
CHAPTER 7: Community Treatment Orders (CTO) ...................................................... 85
7.1 Introduction to Community Treatment Orders ......................................................... 86
7.2 Applicability and Criteria for Issuance of a CTO ................................................. 86
7.3 Competency, Consent to a CTO and Consent to Treatment .............................. 88
7.4 The Process of Treatment and Care Planning.................................................... 90
7.5 Contents of the CTO ........................................................................................... 91
7.6 Forms and Signatures ........................................................................................ 91
7.7 Rights and Notification ........................................................................................ 92
7.8 Application to a Review Panel to Cancel a CTO................................................. 94
7.9 CTO Renewal, Amendment, Cancellation or Expiry ........................................... 95
7.10 Failure to Comply ............................................................................................... 97
7.11 Processes for Apprehension and Conveyance of a Person not Complying with a
CTO .................................................................................................................... 98
7.12 Questions about Community Treatment Orders in Practice................................ 99
7.13 Flowchart: Community Treatment Orders ......................................................... 105
CHAPTER 8: Confidentiality and Access to Information ............................................. 107
8.1 Introduction to the Health Information Act (the “HIA”) ....................................... 107
8.2 The Right to Access Health Information ........................................................... 109
8.3 The Right to Refuse Access to Health Information ........................................... 109
8.4 Using and Disclosing Health Information in a Limited Manner ......................... 110
8.5 Using and Disclosing Health Information without the Patient’s Consent ........... 111
8.6 Disclosure of Health Information with Consent ................................................. 114
8.7 Questions about Access, Use and Disclosure of Health Information in Practice
......................................................................................................................... 115
Classification: Protected A 6
CHAPTER 9: Mental Health Patient Advocate ............................................................ 119
9.1 Jurisdiction........................................................................................................ 120
9.2 Investigations Based on Complaints ................................................................. 120
9.3 Investigations without a Complaint ................................................................... 120
9.4 Rights Advice.................................................................................................... 121
9.5 Notification Requirements................................................................................. 122
9.6 Refusal to Investigate ....................................................................................... 122
9.7 Conduct of Investigation ................................................................................... 123
9.8 Conduct of Investigation; Right to Make Representations ................................ 123
9.9 Conduct of Investigation; Cooperation by the Facility ....................................... 123
9.10 Confidentiality of Information Obtained During the Investigation ...................... 124
9.11 Record of Investigation ..................................................................................... 124
9.12 Reporting at the End of an Investigation ........................................................... 124
9.13 Contact Information .......................................................................................... 124
9.14 Questions about the Mental Health Patient Advocate in Practice ..................... 125
APPENDIX I: Glossary ................................................................................................ 127
APPENDIX II: List of Designated Facilities .................................................................. 133
APPENDIX III: Mental Health Act Forms ..................................................................... 135
APPENDIX IV: Investigations that may occur within Designated Facilities ................. 137
APPENDIX V: Qualified Health Professionals Roles under the Mental Health Act...... 138
Classification: Protected A 7
Information about the Guide
Limits of the Guide
This guide has been written as a resource for healthcare professionals, service
providers in mental health and related agencies, advocacy organizations, peace officers
and other interested parties.
The purpose of the guide is to simplify and summarize key themes and provisions in the
Mental Health Act (Act), and the associated regulations. Other relevant legislation (e.g.,
the Adult Guardianship and Trusteeship Act, the Health Information Act, and the Public
Inquiries Act) are noted. Readers are encouraged to view the legislation directly.
This document is intended as a guide and as general information only and is not
to replace the advice of legal counsel. Examples herein are for illustrative purposes
and should not be viewed as authoritative statements of the law. Readers should
consult legal counsel if in need of legal advice or clarification regarding the application
of the Act. Further, this guide is not intended to replace or supersede internal policies.
Alberta Health Services (AHS) is not liable in any way for actions based on the use of
information contained in this guide.
Material appearing in the Guide to Alberta’s Mental Health Act may be reproduced or
copied in full for education and program development purposes or not-for-profit, non-
commercial activities without permission.
Questions and answers
A series of questions and answers, found at the end of chapters two through nine,
addresses practice issues relevant to both community and hospital settings.
Judge-made law (common law) and legislation continually change over time. This guide
reflects the Mental Health Act and its regulations as well as the legal setting of
designated facilities as of December 2021.
© 2022 Alberta Health Services.
Contact Information
Alberta Health Services invites your comments and suggestions for enhancing the
contents of this document.
Provincial Clinical Excellence
Addiction and Mental Health
Alberta Health Services
10101 Southport Road SW
Calgary, AB T2W 3N2

Classification: Protected A 8
The Alberta Mental Health Act - Introduction
It is estimated that one in three people will have a mental health problem in their
lifetime. This significant health and quality-of-life issue crosses all demographic, cultural
and socio-economic barriers. A study over a three-year period found that “35% of adult
Albertans consulted a physician and were given a mental disorder diagnosis”. The
number of people treated in the community was far greater than those treated by
specialists. Those with the most serious diagnosis (e.g., psychosis) were more likely to
be seen by psychiatrists.
1
Some individuals with the most serious and persistent mental disorders may refuse to
access help or not recognize the need for psychiatric treatment. Refusal to accept care
can cause pain and disruption which may lead to harm for those individuals, their
families, and the community. In order to protect and treat those individuals with serious
mental disorders and to protect the public, legislation has been put in place.
The Act provides the authority, criteria, procedures and timelines for the apprehension,
detention, admission, and treatment of an individual as a formal patient and contains
other provisions that apply to all patients who fall under the Act. In addition, the Act
identifies separate criteria and conditions for supportive treatment of persons living in
the community – including some who are former formal patients. Adults, seniors, and
minors may be admitted as formal patients or subject to a CTO if they meet the criteria
outlined in the Act.
History of Mental Health Legislation in Alberta
Earliest legislation in Alberta was concerned with the safety of society. In 1879 a justice
of the peace could incarcerate those deemed dangerous to be at large, insane and
most likely to be associated with a criminal offence. A jail was the only available
detention centre. By the late 1880s the criteria of dangerousness and suspected
criminality were set aside; a person could be confined to jail or other safe custody for
reasons of insanity alone.
Although the concept of ‘dangerous to be at large’ returned in the Insanity Act of 1907,
important next steps were reflected in the requirement that a qualified medical
practitioner provide evidence before a person could be confined. Additionally, there was
a provision that a judge of the Supreme Court of Alberta could review any committal.
The Insanity Act was renamed the Mental Diseases Act in 1924. Asylums were now
called hospitals, and it was recognized that hospitalized individuals were sick and
1
Slomp, M., Bland, R., Patterson, S., Whittaker, L. (2009). Three-Year Physician Treated Prevalence
Rate of Mental Disorders in Alberta. Canadian Journal Psychiatry, 54(3):199–202.

Classification: Protected A 9
required care and treatment. In 1942, the word insane was replaced by mentally
diseased.
In 1964, all those with a mental disorder came under the same legislation. The first
Mental Health Act of Alberta proposed a more community centered approach to mental
health care. Decisions to admit individuals to hospital were made by physicians, and
time limits to the length of detention were identified. Equally important was the formation
of independent review panels.
With the 1989 Mental Health Act patient rights were aligned with those in the Canadian
Charter of Rights and Freedoms. The provision of care and treatment for formal patients
expanded from provincial psychiatric hospitals to a further 15 designated facilities in
towns and cities across the province. Forensic psychiatry services and facilities were
provided in both Edmonton and Calgary.
Further amendments to the Mental Health Act were proclaimed in two stages on
September 30, 2009 and January 1, 2010, following a lengthy process of consultation
and review.
2
Those amendments broadened the criteria for certification to permit earlier
intervention and treatment, and introduced community treatment orders (CTOs) to
encourage individuals to maintain mental health treatment in the community, ideally
reducing the need for hospitalization. The role of Alberta’s Mental Health Patient
Advocate (Patient Advocate) was expanded to allow the Patient Advocate to respond to
and investigate complaints when a person was detained under one admission certificate
and to assist persons subject to CTOs. Previously, the Patient Advocate could intervene
only if a person had formal patient status, that is, had two admission or two renewal
certificates requiring them to be detained in a designated facility.
Recent amendments to the Act were proclaimed in force in stages: September 30,
2020, and March 31, 2021. The amendments made changes to the longstanding
definition of “mental disorder” and introduced two new terms: qualified health
professional, and secure location. Treatment is now defined and the concept of
treatment plans is introduced. Additional changes are highlighted below and explained
in further detail throughout the guide.
Definition of Mental Disorder
Mental disorder is defined as a substantial disorder of thought, mood, perception,
orientation, or memory that grossly impairs judgment, behaviour, capacity to recognize
reality, or ability to meet the ordinary demands of life, but does not include a disorder in
which the resulting impairment is persistent and is caused solely by an acquired or
2
The history and purpose of these amendments is explained in: M. Marshall, Everything You Want to
Know about Changes to the Mental Health Act in Alberta, Health Law Review (2010), Vol. 19, No. 1.

Classification: Protected A 10
congenital irreversible brain injury. The change to the definition is supported by the
following definitions in section 2.1 of the Mental Health Regulation:
(a) “irreversible brain injury” means a permanent disruption to the
baseline function of the brain or to the structure of the brain caused
or likely caused by an identifiable or probable
(i) acute external action, including trauma, or
(ii) pathophysiological event within the body, including an acute
hypoxic event,
but does not include a permanent disruption caused or likely
caused by a neurodegenerative disorder;
(b) “persistent” means stable and unlikely to improve as a result of
treatment.
Qualified Health Professional
Qualified health professional means a physician or nurse practitioner or a person who is
registered under section 33(1)(a) of the Health Professions Act as a member of a health
profession or of a category within a health profession designated by the Mental Health
Act regulations for the purposes of all or part of the Mental Health Act. The Minister may
designate in the future other qualified health professionals under the Mental Health Act
regulations, but at this time, a qualified health professional is a psychiatrist, physician,
or nurse practitioner. The role of a qualified health professional is set out in Appendix V.
Secure Location
Secure locations are introduced in section 13.1 of the Act and are designated by
ministerial order. Peace officers may convey an individual under a Form 8 - Warrant
(section 10 of the Act) or under a Form 10 - Statement of Peace Officer on
Apprehension (section 12 of the Act) to a secure location (or a designated facility) for
assessment and examination. Only the initial assessment and examination takes place
at a secure location; this assessment is to occur as soon as possible by a qualified
health professional (physician or nurse practitioner). This guide will be updated when
secure locations have been designated by the Minister and are an option for
assessment and examination.
Cancellation Certificate
Form 2.1 – Cancellation of Admission Certificate or Renewal Certificate is introduced in
section 31(4) and section 3.1 of the Mental Health Act Forms and Designation
Regulation. The physician who cancels admission or renewal certificates of a formal
Classification: Protected A 11
patient is required to complete Form 2.1 – Cancellation of Admission Certificates or
Renewal Certificates.
Virtual Health
Assessments and examinations of persons in facilities may be done by video
conference, provided the use of technology for the assessment and examination is
reasonable in the circumstances (section 13.2 of the Act). Such examinations are
already explicitly provided for in the CTO context; the above amendment expressly
permits examinations using video conference for all examinations that take place at a
facility.
Revised Criteria for Admission Certificates and Renewal
Certificates
The criteria for admission and renewal certificates have been amended to provide that
the person must be able to benefit from treatment for their mental disorder; and the
person is within a reasonable time, likely to cause harm to others or to suffer negative
effects, including substantial mental or physical deterioration or serious physical
impairment, as a result of or related to the mental disorder.
Reasonable Grounds
A formal patient may now only object to informing the patient’s nearest relative of the
reasons for issuance of certificates, etc., on “reasonable grounds”. In other words, the
formal patient must demonstrate to the board an objective reason to support not
informing the patient’s nearest relative.
• Similarly, formal patients may now object to a qualified health professional informing
the patient’s nearest relative on reasonable grounds for the purposes of a Form 11 -
Certificate of Incompetence to Make Treatment Decisions and the notice of
discharge (sections 27(3) and 32 of the Act).
Note: a formal patient does not require “reasonable grounds” to object to [sections 18(1)
set out additional context and specific sections.]
Revised Responsibilities of Facility Leadership
Facilities that are designated in the regulations may be operated by AHS or Covenant
Health. The Act refers to board responsibilities, and facility leadership assumes those
responsibilities. Newly added responsibilities are listed here:
• Review Admission and Renewal Certificates (section 8.1 of the Act):
Classification: Protected A 12
- The board must ensure admission and renewal certificates issued in respect
of a person, are reviewed as soon as possible upon completion to ensure the
form is complete, issued and provided to the person.
• Treatment Plans (section 9.01 of the Act):
- The board shall ensure that a formal patient is provided with a written,
individualized treatment plan within a month of their second admission
certificate being issued.
- There are specific elements that must be included in the treatment plan,
including: the type of treatment expected to be provided, the criteria on which
a formal patient would be released, and the criteria for privileges such as a
leave of absence to be granted.
- Treatment is defined as anything that is done for a therapeutic, preventative,
or other health-related purpose, including the implementation of a treatment
plan.
• Additional Duties Towards Patients (section 14 of the Act):
- There is a requirement to inform formal patients of the right to counsel.
- The written statement provided to the patient must also specify the steps for
the patient to follow to obtain free legal services, the function of the Patient
Advocate, patients’ rights to contact the Patient Advocate, and the right to
obtain timely and free access to medical records for the purposes of a hearing
before a review panel or appeal to the Court of King’s Bench.
- The board shall inquire with the formal patient to determine whether the
patient wishes to be contacted by the Patient Advocate, and, if so, the board
shall notify the Patient Advocate and provide a copy of the admission/renewal
certificates and a summary of the information provided to the formal patient
under section 14 of the Act.
• Access to Records (section 14(6) of the Act):
- When a formal patient applies to the review panel or to the Court of King’s
Bench, the board shall provide the patient a copy of the relevant medical
records in advance of the hearing or appeal, free of charge and as soon as
practicable.
• Form 6 - Memorandum of Transfer to Another Facility (section 22(1.1) of the Act):
- Form 6 - Memorandum of Transfer to Another Facility is no longer required to
transfer a formal patient between two facilities operated by a single regional
health authority, or between two facilities operated by a contracted service
Classification: Protected A 13
provider of a regional health authority. This form needs to be completed only
when a patient is being transferred from
(a) a designated AHS facility to the Grey Nuns Community Hospital,
Misericordia Community Hospital or Villa Caritas, or
(b) the Grey Nuns Community Hospital, Misericordia Community Hospital
or Villa Caritas to a designated AHS facility.
New Reporting Requirement
AHS shall, on an annual basis, provide the Minister of Health a written report assessing
the completion, accuracy and use of admission certificates and renewal certificates, as
well as any other matter requested by the Minister. The Minister may also request a
report on another basis or schedule (section 49.1 of the Act).
Community Treatment Orders (CTOs)
• CTOs may be issued where a person is likely to cause harm to others or to suffer
negative effects, including substantial mental or physical deterioration or serious
physical impairment, as a result of or related to the mental disorder (section
9.1(b)(iii) of the Act).
• Individuals may now apply to a review panel for an order that the board issue a CTO
(section 38(1)(b) of the Act).
• The timelines between two qualified health professionals completing separate
examinations and issuing a CTO renewal has increased from 72 hours to 7 days
(section 9.3(4) of the Act). Timelines for the initial CTO issuance remain unchanged.
• Amendments to the Community Treatment Order Regulation reflect the amendments
to the CTO provisions in the Act.
- Examination by video conference is expressly permitted for the purposes of
renewals under section 9.3 of the Act (section 2 of the Community Treatment
Order Regulation).
- The regulation reiterates that when a review panel makes an order for a
board to issue a CTO in respect of a formal patient, the CTO is to be issued in
a reasonable amount of time in accordance with section 9.1 of the Act
(section 2.1 of the Community Treatment Order Regulation).
- The nearest relative of a person subject to a CTO is now prescribed by the
regulation as a person to whom a written statement (first page of Forms 19,
20 and 21) and copy of an issued, amended, or renewed CTO must be given
under section 14(1.1) of the Act, unless the person objects on reasonable
grounds (section 7(3) of the Community Treatment Order Regulation).
Classification: Protected A 14
Mental Health Review Panels (review panels)
- A review panel may order a further psychiatric assessment and examination
of the formal patient or person subject to a CTO for the purpose of informing
its decision on an application (section 40.1 of the Act).
- Individuals may now apply to a review panel for an order that the board issue
a CTO (section 38(1)(b) of the Act).
- Individuals now have 30 days, instead of 14 days, to appeal a review panel’s
order to the Court of King’s Bench (section 43(1) of the Act).
Mental Health Patient Advocate (Patient Advocate)
Additional responsibilities are outlined for the Patient Advocate including but not limited
to: a) contacting formal patients who have asked to be contacted; b) providing
information to formal patients, formal patients’ guardians; and c) ensuring all information
required to be provided by the board was provided (section 45(1.1) of the Act).
The Mental Health Patient Advocate Regulation, AR 148/2004 is repealed and replaced
by Mental Health Patient Advocate Regulation, AR 173/2020.
- An investigation may now be initiated by the Patient Advocate into any matter
under the Act relating to a patient, with or without the patient’s consent
(section 4(1) of the Mental Health Patient Advocate Regulation).
- Previously, without the patient’s consent, the Patient Advocate could only
initiate an investigation into various procedures of a facility (e.g., procedures
related to the admission of persons detained under the Act, procedures for
informing patients of their rights, etc.).
- If the Patient Advocate determines it is more appropriate for an investigation
to be carried out by another committee, body, person or entity, the Patient
Advocate may refuse to investigate or cease to investigate a matter (section
9(1)(d) of the Mental Health Patient Advocate Regulation).
- The Patient Advocate may request in writing from the facility, board, regional
health authority or “issuing qualified health professional” any policy, directive,
medical record, or other record relating to a patient subject to an investigation
or to whom an investigation relates, and the documents requested must be
provided to the Patient Advocate within a reasonable time (section 11 of the
Mental Health Patient Advocate Regulation). The “issuing qualified health
professional” is defined to mean the qualified health professional who last
issued, renewed, or amended a CTO or issued an apprehension order
(section 1(c) of the Mental Health Patient Advocate Regulation).
Classification: Protected A 15
Protection of Individual Rights within the Mental Health Act
Whether an individual is involuntarily admitted or issued a CTO, the Act protects their
rights by identifying what those rights are and directing that those rights are made
known to the individual - and others who may advocate for them - in a timely manner.
Safeguards for patients include, for example, the right to know why they are being
detained, the right to notify others about their detention, and the right to apply to a
review panel to review or cancel certificates and CTOs. Patient rights also include the
right to access legal counsel and the right to appeal review panel decisions to the Court
of King’s Bench. The Act provides patients who are subject to one or two admission or
renewal certificates or a CTO, and those acting on their behalf, with the right to contact
the Patient Advocate for rights information, support and to investigate concerns or a
complaint.
Protection of patient rights goes hand in hand with treating the patient respectfully. Care
and treatment not only provide safety in times of crisis but also reflect ongoing
compassion for the patient and their circumstances. Finally, healthcare professionals
and mental health service providers should involve the patient in treatment planning to
the extent possible, offering the patient support for recovery and hope for the future.
This guide is divided into chapters that reflect the primary areas dealt with in the
Act and regulations:
- the authority and mechanisms to apprehend and convey for examination
(Chapter 2),
- criteria for admission and detention as a formal, involuntary patient (Chapter
3),
- a formal patient’s rights while detained in a designated facility, including to
apply for review of decisions about their detention and treatment (Chapter 4),
- the function of review panels to respond to applications (Chapter 5),
- determining a person’s capacity to make treatment decisions, and appointing
another individual to act on their behalf if the person lacks capacity (Chapter
6),
- provisions for persons who are subject to community treatment orders
(Chapter 7),
- confidentiality and access to health information (Chapter 8), and
- the powers and duties of the Mental Health Patient Advocate (Chapter 9).
Classification: Protected A 16
The Meaning of “the board” in the Act
In this guide, there are citations from the Act which reference “the board” (e.g., section
14(1)(b) of the Act). When the Act imposes a duty on or grants a power to the “board”,
in practice this has likely been delegated to an employee or physician within the facility,
depending on the circumstances. Readers of the guide are encouraged to check with
management in the facility to determine to whom a particular responsibility or power has
been delegated.

Classification: Protected A 17
CHAPTER 1: Designated Facilities
This chapter will cover
what are facilities,
who can be admitted to a designated facility,
how forensic patients are admitted to designated facilities,
how to manage a complaint at a designated facility, and
responsibilities of the board/facility leadership.
1.1 Introduction to Facilities
Definition of facilities
Facilities are places (or parts thereof) that have been designated in the Mental Health
Act Forms and Designation Regulation as ‘facilities’ for the purpose of the Act. In
practice, the term “designated facilities” refers to inpatient health facilities which have
been authorized by the Minister of Health as the only places that can admit and detain
formal or involuntary patients under the Act. There are many healthcare facilities in
Alberta but only a limited number are designated facilities. A list of designated facilities
as of December 2021 is in Appendix II (section 15.2 of the Mental Health Act Forms and
Designation Regulation, Alta Reg 136/2004).
In the Mental Health Act Forms and Designation Regulation, three types of facilities are
listed, however throughout this guide any references to “facility” will refer to the ones
listed in 15.2(1), not necessarily to sections 15.2(2) and (3).
• Section 15.2(1) of the Mental Health Act Forms and Designation Regulation
are designated as facilities for the purposes of section 1(1)(d) of the Act.
• Section 15.2(2) of the Mental Health Act Forms and Designation Regulation
are designated as facilities for the purposes of section 1(1)(d) of the Act, only
for the purposes of section 13 of the Act.
• Section 15.2(3) of the Mental Health Act Forms and Designation Regulation
are designated as facilities for the purposes of section 1(1)(d) of the Act,
except for the purposes of sections 4(1)(a), 9.6, 10, 12 and 24 of the Act.
Voluntary Patients in Designated Facilities
Classification: Protected A 18
1.2 Voluntary Patients in Designated Facilities
Designated facilities may admit patients who present for mental health assessment and
voluntarily accept admission and psychiatric treatment. This is often the case in urban
centres where the acute care hospitals offering psychiatric care are designated facilities.
Many people admitted to hospital for psychiatric care and treatment have
sought help of their own volition. For example, individuals or family
members may make an appointment with a family physician or psychiatrist
when ‘something is wrong”. Alternatively, they may have accessed help at
a community clinic or a local emergency department.
In the course of the assessment interview with the physician and
healthcare team, the person and/or family member relays changes in the
way the person is functioning, thinking, feeling, or behaving. The person
recognizes the need for help and is willing to accept it. The team assesses
safety issues and the availability of support, as well as the person’s ability
to understand and carry out treatment suggestions.
Depending upon the severity of the symptoms and the amount of support
available in the family and community, the person might be admitted to
hospital voluntarily, discharged from the local emergency department for
follow-up treatment in the community, and/or continue seeing their family
physician or psychiatrist. If admitted voluntarily, the patient would be able
to discharge themselves at any time.
1.3 Formal Patients in Designated Facilities
A person becomes a formal patient when admitted involuntarily and detained in a
designated facility by the issuance of two admission or renewal certificates. Qualified
health professionals are guided by the Act, which contains the criteria that must be met
in order to involuntarily detain a person in a designated facility.
1.4 Minors in Designated Facilities
The Act makes no age distinctions regarding detention in designated facilities. In
Alberta, a minor (defined as anyone under the age of 18 years in section 28(1)(ii) of the
Interpretation Act) as well as adults may be admitted as formal patients when they meet
the four criteria for admission under the Act.
In addition, minors may also be admitted as voluntary patients, usually with the consent
of their parents or guardians or pursuant to the authority of legislation (for example, the
Child, Youth and Family Enhancement Act).
Classification: Protected A 19
1.5 Forensic Patients in Designated Facilities
When a person is remanded to custody for observation or detained for treatment under
the Criminal Code (Canada) or the Youth Criminal Justice Act (Canada) that person can
be admitted to one of the two designated facilities in Alberta authorized to admit these
individuals for examination, treatment, detention and discharge in accordance with the
law (section 13 of the Act, and section 15.2(2) of the Mental Health Act Forms and
Designation Regulation) (see Appendix III).
1.6 Managing Complaints arising within a Designated Facility
Complaints about designated facilities should be addressed with a member of the
treatment team so those caring for the patient are aware that a concern or problem
exists. This process can result in a timely response to the need; for example, providing
additional or clarifying information, support, or corrective action. Patients, their agents,
guardians, and/or families can also take complaints and suggestions to the facility
administration or Patient Relations Department within AHS or Covenant Health. In
addition, patients under one or two admission or renewal certificates, or those acting on
their behalf, have access to the Patient Advocate for information, support, or
investigation of complaints.
As well, the Office of the Alberta Ombudsman and Protection for Persons in Care are
able to conduct investigations concerning designated facilities (see Appendix IV).
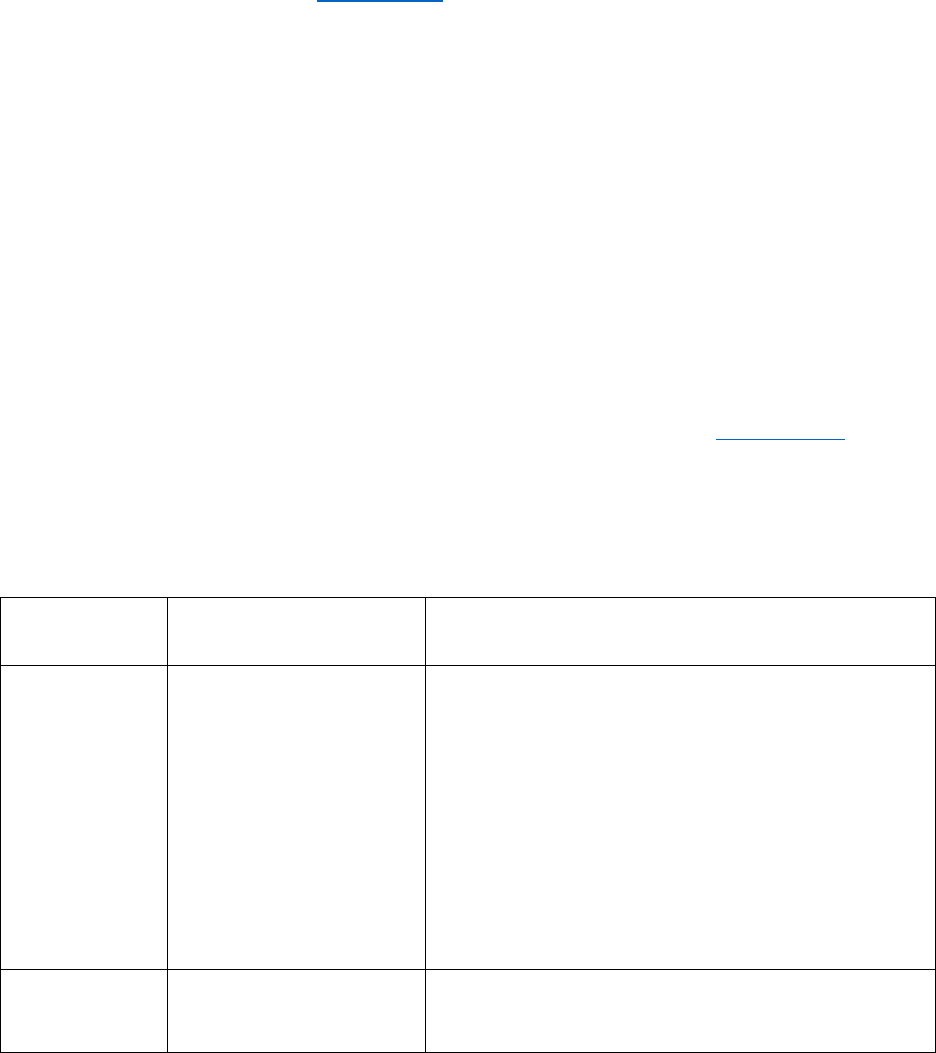
1.7 Responsibilities of the Board / Facility Leadership
The board or facility leadership has been given a number of responsibilities under the
Act, including the ones noted in the chart below.
MHA
Section
General Area
Duty of the Board / Facility Leadership
1(1)(h)(ii)
Designation of
“nearest relative”
The board may designate in writing any adult
person to act as the nearest relative if there is
no nearest relative within any description in
subclause (i) of the definition (e.g., family
member) or if, in the opinion of the board, the
nearest relative determined under subclause
(i) would not act or is not acting in the best
interest of the formal patient or the person
who is subject to a community treatment
order.
5(1)
Examination of
person detained
When a person is conveyed to a facility under
section 10 of the Act (warrant for
Classification: Protected A 20
MHA
Section
General Area
Duty of the Board / Facility Leadership
apprehension by a provincial court judge),
section 12 of the Act (apprehension by a
peace officer) or section 24 of the Act
(transfer into Alberta),or is detained in a
facility pursuant to one admission certificate,
the board of the facility shall ensure that the
person is examined as soon as possible by a
qualified health professional.
8.1
Review and provision
of admission
certificates, renewal
certificates
The board must ensure admission and
renewal certificates issued in respect of a
person are reviewed as soon as possible
upon completion to ensure the form is
complete, issued and provided to the person.
9.01
Treatment Plan
The board shall ensure that a formal patient
is provided with a written, individualized
treatment plan within a month of their second
admission certificate being issued. There are
specific elements that must be included in the
treatment plan, including: the type of
treatment expected to be provided, the
criteria on which formal patient would be
released, and the criteria for privileges such
as a leave of absence to be granted.
Treatment is defined as anything that is done
for a therapeutic, preventative, or other
health-related purpose, including the
implementation of a treatment plan (section
1(1)(p.2) of the Act).
14(1)(a)
Duties toward
patients – Information
When two admission or renewal certificates
are issued with respect to a patient, the board
must inform the formal patient and make a
reasonable effort to inform the patient’s
guardian, if any, and, unless the patient
objects on reasonable grounds, the patient’s
nearest relative, of
(i) the reason, in simple language, for the
issuance of the admission certificates or
renewal certificates,
(ii) the patient’s right to apply to the review
panel for cancellation of the admission
certificates or renewal certificates or for an
Classification: Protected A 21
MHA
Section
General Area
Duty of the Board / Facility Leadership
order for the board to issue a community
treatment order, and
(iii) the patient’s right to legal counsel.
14(1)(b)
Duties toward
patients – Written
Statement
The board must give the formal patient, the
patient’s guardian, if any, one person
designated by the patient, and unless the
patient objects on reasonable grounds, the
patient’s nearest relative a written statement.
The written statement must include the
information specified in section 14(1)(a) of
the Act.
The written statement provided to the patient
must also specify the steps for the patient to
follow to obtain free legal services, the
function of the Mental Health Patient
Advocate (Patient Advocate), patients’ rights
to contact the Patient Advocate, and the right
to obtain timely and free access to medical
records for the purposes of a hearing or an
appeal.
14(1)(c)
Duties toward
patients – Copies of
Documents
The board must provide the patient, the
patient’s guardian, if any, one person
designated by the patient and, unless the
patient objects on reasonable grounds, the
patient’s nearest relative with copies of the
admission certificates or renewal certificates,
and a summary of the assessment made of
the patient’s competence to make treatment
decisions.
14(1)(d)
Duties toward
patients – Contact by
Mental Health Patient
Advocate
The board must inquire with the formal
patient to determine whether the patient
wishes to be contacted by the Patient
Advocate, and, if so, the board must notify
the Patient Advocate and provide the Patient
Advocate with a copy of the
admission/renewal certificates and a
summary of the information provided to the
formal patient under section 14 of the Act.
14(2)
Duties toward
patients – Interpreter
In the event of language difficulty, the board
must obtain a suitable interpreter and provide
the information and the written statement
referred to in section 14(1) of the Act in the
Classification: Protected A 22
MHA
Section
General Area
Duty of the Board / Facility Leadership
language spoken by the formal patient or the
patient’s guardian.
14(3)
Duties toward
patients – Facilitate
application
In addition to giving a written statement
pursuant to section 14 of the Act, the board
shall do any other things the board considers
expedient to facilitate the submission of an
application to the review panel.
14(4)
Duties toward
patients - Information
for person designated
by formal patient
If a formal patient has designated another
person to receive notices, the board shall
also mail a copy of all notices and information
required to be given to the patient to the
person designated at the address provided
by the patient.
14(6)
Duties toward
patients - Provision of
Medical Records
When a formal patient applies to a review
panel or the Court of King’s Bench, the board
shall provide the patient a copy of the
relevant medical records in advance of the
hearing, free of charge and as soon as
practicable.
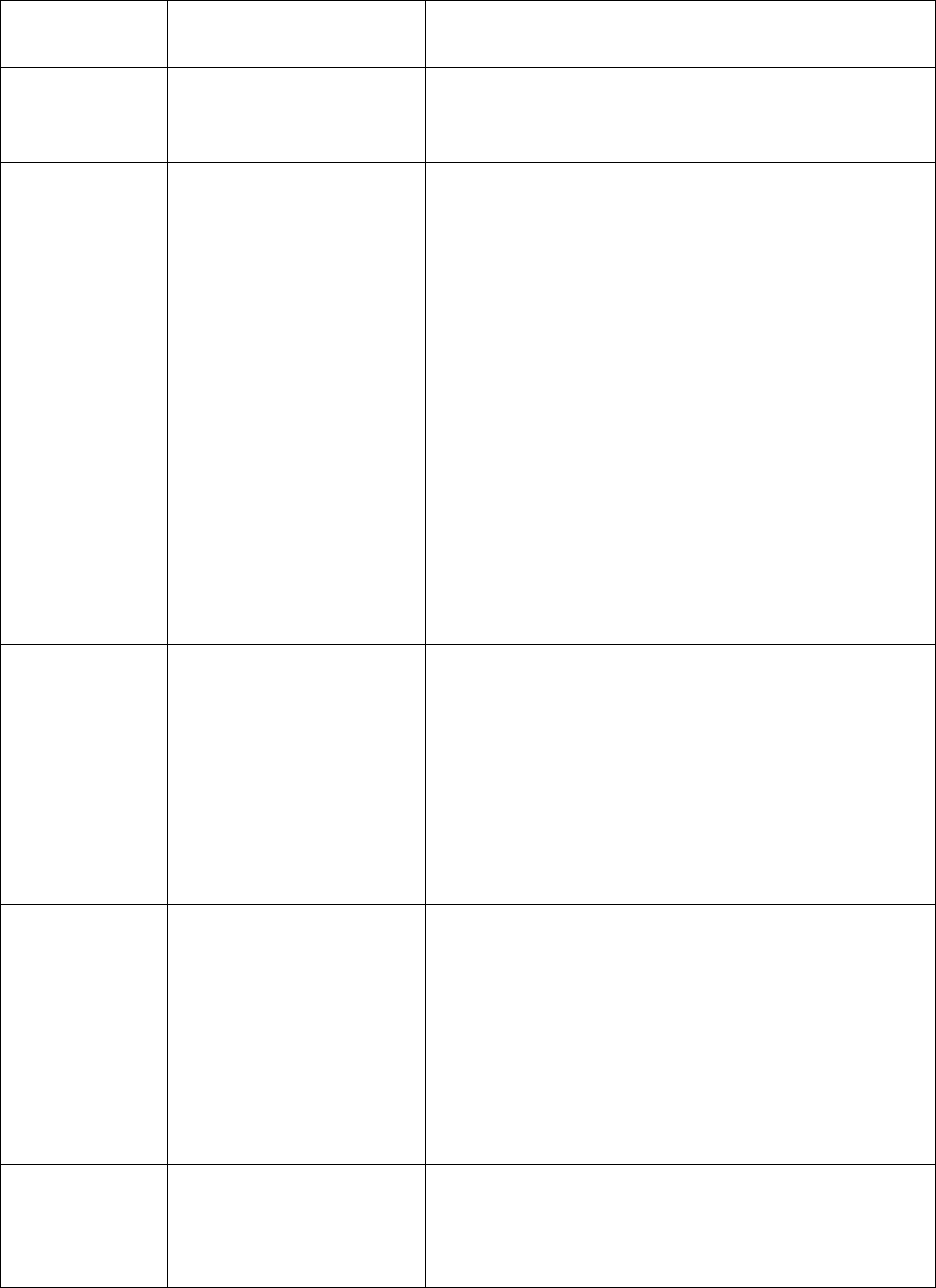
18(1)
Refusal of Admission
to facility – Provision
of Information
When any person is conveyed to a facility
pursuant to one admission certificate and
another admission certificate is not issued
with respect to that person, the board shall
inform the person and, if the person does not
object, the referring source, of the reasons
why another certificate was not issued and
may refer the person to another facility or
service, in which case the referring source
shall, unless the person objects, be informed
of any alternative arrangements made.
19(1)
Treatment and
Security of Patients –
Provision of
Diagnostic and
Treatment Services
On the admission of a patient to a facility, the
board of the facility shall provide the
diagnostic and treatment services that the
patient is in need of and that the staff of the
facility is capable of providing and able to
provide.
19(2)
Treatment and
Security of Patients –
Level of Security
The board of a facility in which a formal
patient is detained shall determine what level
of security is reasonably required for each
patient in view of all the circumstances and
afterwards provide it and review the
Classification: Protected A 23
MHA
Section
General Area
Duty of the Board / Facility Leadership
necessary level of security at intervals of not
more than three months.
20
Leave of Absence
The board may grant a formal patient a leave
of absence from the facility on any terms and
conditions prescribed by the board. The
board may by notice in writing revoke the
leave of absence and recall the patient.
Where the formal patient refuses or neglects
to return to the facility or when the board is
unable to serve a notice in writing, the board
may declare the person to be absent without
leave and issue an order ordering any peace
officer to return the patient to the facility.
22
Transfer to Another
Facility
A board may, if otherwise permitted by law
and arrangements have been made with the
board of another facility, transfer a formal
patient to that facility on completing Form 6 –
Memorandum of Transfer to Another Facility.
Form 6 - Memorandum of Transfer to Another
Facility is not required to transfer from an
AHS facility to AHS facility, or from a
Covenant Health facility to a Covenant Health
facility but continues to be required to transfer
between an AHS facility and a Covenant
Heath facility.
23(1)
Transfer for hospital
treatment
When a formal patient requires hospital
treatment that cannot be provided in the
facility, the board may, if otherwise permitted
by law, transfer the patient to a hospital for
treatment and return the patient to the facility
on the conclusion of the treatment.
27(3)
Competence to make
Treatment Decisions
– Provision of
Information
The board shall give to the formal patient, the
patient’s agent, if any, the patient’s guardian,
if any, and, unless the patient objects on
reasonable grounds, the patient’s nearest
relative a copy of the certificate and written
notice that the patient is entitled to have the
physician’s opinion reviewed by a review
panel if the patient applies for the review by
sending a notice of application to the chair of
the review panel in the prescribed form.
Classification: Protected A 24
MHA
Section
General Area
Duty of the Board / Facility Leadership
31(1)
Cancellation of
certificates
A board must comply with and take any
action necessary to comply with a decision of
a review panel concerning admission
certificates or renewal certificates.
32(1)
Notice of Discharge
When a patient is discharged from a facility,
the board shall, where reasonably possible,
give notice of the discharge
(a) to the patient’s guardian, if any,
(b) to the patient’s nearest relative, unless the
patient being discharged objects on
reasonable grounds, and
(c) to the physician or nurse practitioner who
treats the patient in their ordinary day-to-day
health care needs, if known, along with the
discharge summary, including any
recommendations for treatment,
and, when applicable, shall state in the notice
whether a certificate of incapacity is in effect
under the Public Trustee Act with respect to
the patient.
41(1)
Decision of review
panel
A review panel may order the board to issue
a community treatment order (CTO) in
respect of a patient within a reasonable
amount of time.
42(1)
Onus in review panel
or Court of King’s
Bench hearing
In a hearing before a review panel or the
Court of King’s Bench, the onus is on the
board of the facility in which the patient is
detained to show that
(a) detention is required, and the patient
meets the criteria referred to in sections 2
and 8(1),
(b) the physician’s opinion under section 27 is
correct,
(c) it is in the best interest of the formal
patient to administer treatment in accordance
with section 29, or
(d) the patient should not be returned to a
correctional facility under section 33, as the
case may be.
Classification: Protected A 25
CHAPTER 2: Apprehension and Conveyance to a
Designated Facility; Detention in a Designated
Facility
This chapter will cover
• how to access an examination by a qualified health professional under the Act,
• how a Provincial Court judge, peace officer and qualified health professional
facilitate apprehension and conveyance of a person, including someone not
complying with a CTO, to a designated facility,
• what criteria are necessary for any person, adult or minor to be made a formal
patient,
• what timeframes are allowed for conveyance and apprehension,
• what timeframes are allowed for a qualified health professional’s examination and
detention under one admission certificate at the designated facility,
• what rights a person has when one admission certificate is issued, and
• questions related to apprehension, conveyance, and detention in practice.
2.1 Apprehension, Conveyance and Detention
The terms apprehension, conveyance and detention are used in the Act to describe the
process of seeking out and taking a person to a designated facility for examination by a
qualified health professional. The person can be detained under the Act, and the
examination must be conducted as soon as possible (section 5(1) of the Act).
Common methods of apprehension and conveyance
This section will focus on the three most common routes that lead to a person being
brought to a designated facility for examination to determine whether they meet the
criteria to be admitted as a formal patient.
The authority to apprehend an apparently mentally disordered person can be given by
the following people:
• a qualified health professional using Form 1 - Admission Certificate (section 2 of the
Act),
• a Provincial Court judge using Form 8 - Warrant (section 10 of the Act), or
• a peace officer using Form 10 - Statement of Peace Officer on Apprehension
(section 12 of the Act).
Other methods of apprehension and conveyance
Classification: Protected A 26
A person may also be apprehended and conveyed to a designated facility under the
authority of
• Form 23 - Community Treatment Order Apprehension Order (section 9.6 of the Act),
• Form 4 - Certificate of Transfer into Alberta (section 24(1) of the Act),
• Form 3 – Order to Return a Formal Patient to a Facility (section 20(4) or 21(1) of the
Act),
• an admission certificate issued under section 3 of the Act for a person detained
under the Criminal Code (Canada) or the Youth Criminal Justice Act (Canada) who
has been found
- unfit to stand trial, not criminally responsible because of their mental disorder,
or not guilty by reason of insanity, and
- the person’s detention is about to expire.
2.2 Apprehension and Conveyance by First Admission
Certificate (Form 1 - Admission Certificate)
The initial assessment may occur in the community (e.g., a physician’s office) where the
qualified health professional determines whether the person meets the criteria
necessary for issuing a Form 1 - Admission Certificate under the Act.
The completion of one admission certificate allows time and provides the legal
authority for the individual to be brought to a designated facility. In most
situations a person will be brought by family or friends, or by Emergency Medical
Services, especially in situations where medical support is required. A peace
officer may also bring a person to a designated facility for further examination.
If the admission certificate is completed on the unit or in the emergency department of a
designated facility, the Act permits the person to be detained for a specified amount of
time in order that activities prescribed under the Act may take place.
Four criteria for admission certificate
In order to complete a Form 1 - Admission Certificate the examining qualified health
professional must believe that a person
• is suffering from mental disorder,
• has the potential to benefit from treatment for the mental disorder,
• is, within a reasonable time, likely to cause harm to others or to suffer negative
effects, including substantial mental or physical deterioration or serious physical
impairment, as a result of or related to the mental disorder, and
• is unsuitable for admission to a facility other than as a formal patient.
Classification: Protected A 27
All four criteria must be met.
Definition of “mental disorder”
“Mental disorder” means a substantial disorder of thought, mood, perception,
orientation, or memory that grossly impairs
• judgment,
• behavior,
• capacity to recognize reality, or
• ability to meet the ordinary demands of life (section 1(g) of the Act).
The definition of mental disorder “does not include a disorder in which the resulting
impairment is persistent and is caused solely by an acquired or congenital
irreversible brain injury”. The definitions of “irreversible brain injury” and “persistent”
are set out in section 2.1 of the Mental Health Regulation as follows:
(a) “irreversible brain injury” means a permanent disruption to the
baseline function of the brain or to the structure of the brain caused
or likely caused by an identifiable or probable
(i) acute external action, including trauma, or
(ii) pathophysiological event within the body, including an acute
hypoxic event, but does not include a permanent disruption
caused or likely caused by a neurodegenerative disorder.
(b) “persistent” means stable and unlikely to improve as a result of
treatment.
The meaning of the fourth criterion
“Unsuitable for admission to a facility other than as a formal patient” may mean
that
• there are concerns that the patient would leave hospital abruptly and come to harm if
admitted voluntarily (e.g., be at higher risk for suicide) or
• the person being examined may be considered to lack the mental capacity to
understand and consent to admission and treatment.
Further, this fourth criterion may be met when a competent person – or an incompetent
person’s substitute decision-maker (SDM) – refuses to consent to that person being
admitted to a facility to receive psychiatric treatment.
Classification: Protected A 28
Timeframes for Examination by a Qualified Health Professional;
Issuance of First Admission Certificate
A qualified health professional in the community or a hospital may issue a Form 1 -
Admission Certificate within 24 hours of examining a person (section 2 of the Act).
Once a Form 1 - Admission Certificate has been issued in the community, any person is
allowed 72 hours from the time the Form 1 - Admission Certificate is issued to
apprehend the person named in the certificate and to care for, observe, assess, detain,
control, and convey them to a designated facility (section 4 of the Act).
When a person is detained in a facility under a Form 1 - Admission Certificate, or a
person is conveyed to a facility (under section 10, 12 or 24 of the Act) the detained
person must be examined as soon as possible by a qualified health professional
(section 5(1) of the Act).
When assessing the patient’s mental state, collateral information from
family and friends, community healthcare workers, peace officers and
members of the community may be taken into account. It must be noted
on the Form 1 – Admission Certificate which facts were communicated by
others.
Options following issuance of the first admission certificate
At least one of the admission certificates must be issued by a physician, and at least
one of the admission certificates must be issued by a member of staff of the facility
(section 7(2) of the Act).
If a second admission certificate is not issued within 24 hours of the person’s arrival at
the designated facility, the person can no longer be detained involuntarily and shall be
released (section 5 of the Act). Alternatively, the person may remain as a voluntary
patient. If the first admission certificate is issued at the designated facility, section 5 of
the Act requires that both admission certificates be completed within 24 hours.
2.3 Warrant for Apprehension Issued by a Provincial Court
Judge (Forms 7 & 8)
When a person will not see a physician
Help can be accessed through the Provincial Court by families, caregivers,
healthcare workers and peace officers. This could be an option, for
instance, when a person suffering from a mental disorder stops taking
prescribed medication, appears unable to care for themself, is having a
recurrence of severe symptoms yet refuses to see a physician. This same
Classification: Protected A 29
process can be followed if a person is known to be on a CTO and is not
complying with it. See section 2.6 below for more details.
Section 10 of the Act allows any individual, including a peace officer, to bring
information under oath before a Provincial Court judge by filling out Form 7 -
Information. The closest provincial courthouse can provide direction about where to go
and how to bring a Form 7 - Information before a judge. The process varies in each
geographic area.
Criteria to be met
The individual bringing the information to the judge must believe that the person
referred to in the information is
• suffering from mental disorder, and
• within a reasonable time, likely to cause harm to others or to suffer negative effects,
including substantial mental or physical deterioration or serious physical impairment,
as a result of or related to the mental disorder (section 10(1) of the Act).
Information to relate to a judge
It is necessary for the individual bringing information to the judge to
describe the incident(s) and behavior(s) of the person that are causing
concern. Healthcare workers and families and any other person appearing
before a judge for this application may bring notes to which they can refer.
As well as completing documents, the individual bringing the Form 7 –
Information to the judge should expect to answer questions and discuss
with the judge information related to the person’s previous episodes of
mental illness, any diagnoses, and current medications.
The judge must be satisfied that the above criteria have been met, and that a mental
health examination cannot be arranged in any other way. The judge may then issue a
Form 8 - Warrant. This warrant provides authority for a peace officer to apprehend the
person named in the warrant, to care for, observe, assess, detain, and control while
conveying the person to a designated facility for examination.
2.4 Extension of the Warrant (Form 9 - Extension of Warrant)
The warrant expires 7 days after it is issued by the Provincial Court judge, unless it is
extended under section 11 of the Act for a further 7 days (section 10(7) of the Act).
Such an extension is available only once.
A peace officer may make the application to extend the warrant.
Classification: Protected A 30
• This application may be done by telephone or other means of telecommunication if it
is impracticable for the peace officer to appear personally before the Provincial Court
judge.
• The information on which the application is based must be given under oath and
recorded verbatim.
• The information must include a statement of the circumstances that make it
impracticable for the peace officer to appear personally before the provincial judge.
• The order must be filed with the clerk of the court.
2.5 Apprehension by a Peace Officer (Form 10 - Statement of
Peace Officer on Apprehension)
In the course of their work peace officers encounter people with mental illness - many of
whom are not a danger to others or themselves. Peace officers become involved when
they observe behaviors that are of concern, when they receive requests for assistance
from family or healthcare workers, or complaints from a member of the community.
They intervene under the Act when they are satisfied that the person is apparently a
person suffering from a mental disorder and acting in a manner likely to cause harm to
others or to suffer negative effects, including substantial mental or physical deterioration
or serious physical impairment, as a result of or related to the mental disorder.
Criteria for apprehension using a Form 10 - Statement of Peace
Officer on Apprehension
Section 12 of the Act provides that a peace officer may apprehend and convey a person
to a designated facility for examination when they have reasonable and probable
grounds to believe that a person
• is suffering from mental disorder, and
• is within a reasonable time, likely to cause harm to others or to suffer negative
effects, including substantial mental or physical deterioration or serious physical
impairment, as a result of or related to the mental disorder, and
• should be examined in the interests of the person’s own safety or the safety of
others.
The peace officer must also believe that to delay apprehending an individual by first
bringing information under oath before a Provincial Court judge is dangerous (e.g.,
when imminent risk or extreme behaviours of the individual may justify immediate
apprehension and conveyance to a hospital).
Classification: Protected A 31
When assessing whether the person is suffering from a mental disorder for the purpose
of section 12 of the Act, there is a presumption, in the absence of evidence to the
contrary, that the resulting impairment is not persistent; not caused solely by an
acquired or congenital irreversible brain injury; or not persistent and not caused solely
by an acquired or congenital irreversible brain injury (section 2.2 of the Mental Health
Regulation).
The peace officer may then apprehend the person and, while conveying them to a
designated facility for examination, can care for, observe, assess, detain, and control
the person.
When the peace officer conveys the person to a designated facility, the peace officer
must complete a statement using Form 10 – Statement of Peace Officer on
Apprehension (section 11 of the Mental Health Act Forms and Designation Regulation).
Required information includes the name of the person (if known), the date, time, and
place at which the person was apprehended, and the grounds (relative to the Act) upon
which the person was apprehended.
2.6 Apprehension and Conveyance of a Person not Complying
with a Community Treatment Order (CTO).
There are three processes whereby a peace officer may apprehend and convey a
person not complying with a CTO to a designated facility for examination:
1. By carrying out a CTO apprehension order (Form 23 - Community Treatment
Order Apprehension Order)
• completed and signed by a qualified health professional who, despite efforts to
support the person’s compliance with the CTO, has reasonable grounds to believe
the person subject to a CTO has failed to comply with the CTO,
• Form 23 - Community Treatment Order Apprehension Order gives a peace officer
authority to apprehend the person including the entering of premises and the use of
physical restraint, as well as to take into custody, care for, detain and control the
person during conveyance to a specific facility to be examined (section 9.6(1) of the
Act),
• the qualified health professional must indicate on the apprehension form a specific
facility to which the person must be conveyed,
• the order expires 30 days after being issued (section 9.6(3) of the Act).
2. By carrying out a judge’s Warrant (Form 8 - Warrant)
Classification: Protected A 32
• issued when someone brings information under oath before a judge about a person
subject to a CTO regarding their reasonable and probable grounds to believe the
named person is not complying with their CTO (Form 7 - Information),
• if the judge believes that the person is not complying with their CTO, and an
examination cannot be arranged in any other way, the judge may issue a warrant
(Form 8 - Warrant),
• the warrant gives peace officers the authority to apprehend and convey the named
person to a designated facility for examination (section 10(5) of the Act),
• the warrant to apprehend the person expires in 7 days (section 10(7) of the Act). A
peace officer may under oath request a judge to extend the warrant for a further 7
days (section 11 of the Act). Form 9 - Extension of Warrant is used to extend the
warrant.
3. By acting pursuant to section 12(1) of the Act under peace officer discretion
(Form 10 - Statement of Peace Officer on Apprehension)
In order to apprehend and convey, the peace officer must have reasonable and
probable grounds to believe that
• a person is suffering from a mental disorder,
• is subject to a CTO and is not complying with the CTO,
• the person should be examined in the interests of the person’s own safety or
the safety of others, and
• the circumstances are such that to proceed under section 10 (i.e., judge’s
Warrant) would be dangerous.
2.7 Examination at a designated facility
As soon as practicable and at most within 72 hours of being conveyed to a facility
under Form 23 - Community Treatment Order Apprehension Order, Form 8 - Warrant or
Form 10 - Statement of Peace Officer on Apprehension, the person subject to the CTO
must be examined by two qualified health professionals, one of whom must be a
psychiatrist. Under section 9.6(4) of the Act, the two qualified health professionals must
each decide whether
• the CTO should be cancelled, and the person should be released without being
subject to the CTO,
• the CTO should continue, amended as necessary, or
Classification: Protected A 33
• the CTO should be cancelled, and the person should become a formal patient, with
admission certificates issued (Form 24 - Community Treatment Order Examination
on Apprehension).
2.8 Questions about Apprehension, Conveyance and Detention
in Practice
1. Is it legally permissible for a qualified health professional to examine a person
at a designated facility by way of video conference in order to issue the first
admission certificate under the Act?
Yes. Assessments and examinations of persons at designated facilities may be done by
video conference, provided the use of technology for the assessment and examination
is reasonable in the circumstances (section 13.2 of the Act).
2. Can a person under one admission certificate contact the Mental Health
Patient Advocate (the Patient Advocate)?
Yes. The Patient Advocate is able to investigate complaints and provide rights advice to
patients who are or have been subject to one or two admission certificates.
3. Can an admission certificate be issued for a person who is intoxicated or
impaired by drugs or alcohol?
Yes. When a qualified health professional believes the person they have examined
meets all four criteria necessary for the issuance of an admission certificate, the
qualified health professional can complete a first admission certificate and advise the
person that they are being detained for up to 24 hours from time of arrival at a
designated facility.
For example, disorientation, confusion, safety concerns, lack of judgment
or insight and reluctance to accept help are only some of the concerns
with an individual who is acutely intoxicated or impaired which may make
them unsuitable for care except under the Act.
4. Is a peace officer required to complete a Form 10 - Statement of Peace Officer
on Apprehension when they bring a person believed non-compliant with a
CTO to a designated facility for examination under the authority of a Form 23 -
Community Treatment Order Apprehension Order or Form 8 - Warrant?
No. Duplicate forms are not required. Each one of these three processes, whether Form
8 - Warrant (section 10), or Form 23 - Community Treatment Order Apprehension Order
(section 9.6), or Form 10 - Statement of Peace Officer on Apprehension (section 12),
gives a peace officer authority to apprehend and convey a person subject to, and
believed non-compliant with, a CTO to a facility for examination.
Classification: Protected A 34
5. Is the peace officer required to leave the Form 10 - Statement of Peace Officer
on Apprehension at the designated facility?
Yes. The Form 10 - Statement of Peace Officer on Apprehension is completed and
signed by the peace officer and the copy of the original is left with admitting/triage
personnel at the designated facility for inclusion in the person’s health record
(section 12(3) of the Act).
6. Why is it important for Emergency Department staff to note the time of arrival
of any patient coming in under a Form 1 - Admission Certificate, Form 8 -
Warrant, Form 9 - Extension of Warrant or Form 10 - Statement of Peace
Officer on Apprehension)?
Staff must document the time of arrival at the designated facility in order that the
qualified health professionals (whether in the emergency department or an inpatient
unit) can work in compliance with the timeframes provided in the Act. The 24-hour
timeframe allowed for examination and completion of admission certificate(s) is
determined from the time of the person’s arrival at the designated facility (section 5 of
the Act).
7. Are individuals with Fetal Alcohol Spectrum Disorders or Pervasive
Developmental Disorders, eligible for admission as a formal patient?
Yes; the specific diagnosis is not the issue. If a person meets all four criteria for
certification under the Act, they may be admitted as a formal patient. The revised
definition of mental disorder specifies that it does not include a disorder in which the
resulting impairment is persistent and is caused solely by an acquired or congenital
irreversible brain injury.
8. Who is responsible to repatriate the person following discharge at a facility?
It is the responsibility of the designated facility where the person was conveyed for
examination to repatriate them home if they are not admitted to the designated facility
as a patient following examination.
Classification: Protected A 35
CHAPTER 3: Admission and Detention
This chapter will cover
• how to admit and detain a person as a formal patient using two admission
certificates,
• what information is required on an admission certificate,
• how and why treatment plans are developed
• how the detention period is extended by issuing renewal certificates,
• how to remand a person to a designated facility for examination,
• how the formal patient can apply for cancellation of admission or renewal
certificates,
• how formal patients may be granted a leave of absence while hospitalized,
• how formal patients are transferred between designated facilities,
• when notification of discharge from a designated facility is required,
• questions about admission and detention in practice, and
• a review of the Flowchart and Key Points for Formal Patient Certification.
3.1 Second Admission Certificate
Upon arrival at a facility, two qualified health professionals must examine a person and
complete two admission certificates within 24 hours of time, in order for the person to
be detained as a formal patient (section 5(2) of the Act).
If brought to a facility under one admission certificate (Form 1 - Admission Certificate), a
second admission certificate must be signed within 24 hours of the person’s arrival at
the designated facility, or the person must be released on the expiry of 24 hours
(section 5(3) of the Act).
At least one of the admission certificates must be issued by a physician and at least one
of the admission certificates must be issued by a member of the staff of the facility
(section 7(2) of the Act).
In practice, a person may be admitted to an inpatient unit from the
emergency department with one admission certificate, but, in order for the
person to be detained as a formal patient, a second admission certificate
must be issued in the timelines stated above.
These two admission certificates are sufficient authority to diagnose, care for, observe,
assess, treat, detain, and control the person in a facility for 1 month after the second
admission certificate is issued (section 7(1) of the Act).
Refusal of admission to a facility
Classification: Protected A 36
If a person is conveyed to a facility under one admission certificate and a second
admission certificate is not issued, the board must inform the patient, and (if the patient
does not object) also inform the referring source - the qualified health professional who
issued the first admission certificate - of the reasons why a second certificate was not
issued. The person may be referred to another facility or service, and if so, unless the
person objects, this information shall be provided to the referral source (section 18(1) of
the Act).
Responsibility for informing the issuer of the first admission
certificate that the person was not certified
Section 18 gives this responsibility to the board; however, in clinical practice this
responsibility has been delegated to facility staff or physicians. The qualified health
professional who assessed the person will be most aware of the reasons for not issuing
a second certificate and certifying a patient. It may be appropriate that the second
qualified health professional communicate with the qualified health professional who
issued the first certificate. Other necessary information to impart includes any
arrangements or recommendations made for follow-up care.
3.2 Contents of Admission Certificates
Mental Health Act certificates are legal documents. It is essential that they be legible
and accessible to the patient and those acting on their behalf. Both admission
certificates must include the
• name of the person,
• name and business address of the qualified health professional signing the
admission certificate,
• date and time when the qualified health professional’s examination was conducted,
• facts for each of the following four criteria leading to the qualified health
professional’s opinion that the person
- is suffering from mental disorder,
- has the potential to benefit from treatment for the mental disorder,
- is, within a reasonable time, likely to cause harm to others or to suffer
negative effects, including substantial mental or physical deterioration or
serious physical impairment, as a result of or related to the mental disorder,
and
- is unsuitable for admission to a facility other than as a formal patient,
Classification: Protected A 37
• name of place where the person was examined, or the location of the person who
was examined if the examination takes place by video conference,
• name and address of the facility to which the person is to be conveyed to be
examined, if the person is not in a facility,
• date and time the certificate was issued, and
• signature and printed name of the qualified health professional who performed the
examination.
Certificates are to be reviewed for completion (section 8.1 of the Act). This requirement
can be met by having a staff member (not required to be a physician or a nurse
practitioner) at a designated facility review the certificates for completeness. At the time
of this writing, completeness is considered to be legible information being present on all
parts of the certificate where information is required.
3.3 How and Why Treatment Plans are Developed?
Section 9.01 of the Act sets out the requirements of the treatment plan, including that
the individualized treatment plan must:
• be provided in written form no later than one month after the issuance of the 2nd
Admission Certificate (Form 1),
• set out the type of treatment expected to be provided to the formal patient,
• set out the criteria to grant privileges and passes to the formal patient, and
• set out the criteria required to end status as a formal patient.
Alberta Health Services (AHS) has created the Treatment Plan for a Formal Patient for
provincial use to meet the requirements of section 9.01 of the Act.
3.4 Extending the Detention Period by Renewal Certificates
If a formal patient requires hospitalization beyond the period of 1 month from the date
the second admission certificate was issued, there is a mechanism under the Act to
extend the period of detention.
It requires two qualified health professionals, one of whom must be a psychiatrist and
one of whom must be a member of the facility’s staff, to separately examine the formal
patient and issue a renewal certificate before the expiry date of the second admission
certificate (section 8(2) of the Act). When the patient meets the criteria for continued
certification the qualified health professionals may extend the term of detention by each
issuing a renewal certificate within 24 hours after their examination using Form 2 -
Renewal Certificate (section 8(1) of the Act).
Criteria for renewal certificates
Classification: Protected A 38
The two qualified health professionals must separately believe that the formal patient
• is suffering from mental disorder,
• has the potential to benefit from treatment for the mental disorder,
• is, within a reasonable time, likely to cause harm to others or to suffer negative
effects, including substantial mental or physical deterioration or serious physical
impairment, as a result of or related to the mental disorder, and
• is unsuitable for admission to a facility other than as a formal patient.
Section 8(3) provides for use of renewal certificates (Form 2 - Renewal Certificate) to
extend the period of detention
• in the first instance of renewal, for 1 month,
• in the second instance, a further month,
• in the third and subsequent instances, 6 additional months.
The Act does not specify that the renewal certificates have to be
completed within 24 hours of each other. In practice, both renewal
certificates must be issued before the date and time of expiry of the
second certificate (sections 7 and 8 of the Act).
3.5 Completion of Forms
The board must ensure admission and renewal certificates issued in respect of a person
are reviewed as soon as possible upon completion to ensure the form is complete,
issued and provided to the person (section 8.1 of the Act).
Missing information and corrective action
Certificates are legal documents; it is important that they are filled out completely and
accurately. If information is missing on a certificate, or added after the certificate is
signed, it is possible that the certificate will not be valid. Healthcare providers may
address specific questions to their organization’s internal legal services.
3.6 Admission and Detention Arising from an Arrest for Criminal
Charges
When a person suffering from a mental disorder is arrested on a criminal charge, one or
more of the following actions may occur:
• a person can be released outright or released on bail,
• a person capable of consenting to treatment can be treated voluntarily in a remand
centre, while awaiting court proceedings,
Classification: Protected A 39
• depending upon the nature of the criminal charges, the person may be released on
bail, with the requirement to participate in outpatient mental health services,
• an examining qualified health professional may believe that the person meets the
requirements to be involuntarily detained in a designated facility, and may issue a
first admission certificate. The person will then be conveyed to a designated facility,
where they will be assessed by another qualified health professional for their
eligibility relative to a second admission certificate,
• depending on the nature of the criminal charges, the Crown Prosecutor may redirect
the person to the Provincial Diversion Program,
• a court can order the person to be conveyed to a designated forensic facility for
assessment regarding whether the person is fit to stand trial. During the assessment
period, the person can be treated voluntarily or be detained under the Mental Health
Act as an involuntary patient,
• a court can order that a person be detained in a facility and order involuntary
treatment to enable the person to become fit to stand trial.
A person serving a sentence in a provincial correctional facility (less than 2 years’
incarceration) or a federal penitentiary (2 years’ or more incarceration) may be
transferred to a designated forensic facility.
• An assessment will be conducted, and the person may be returned to the place
where they were originally incarcerated.
• Alternatively, the person may be admitted involuntarily pursuant to admission or
renewal certificates and serve the remainder of their sentence in a designated
forensic facility.
A person found by a court to be Not Criminally Responsible due to a Mental Disorder
(NCRMD) will be sent to a forensic psychiatric unit until they are released by the Alberta
Review Board.
3.7 Application to Cancel Certification and Detention
Under the Constitution Act, 1982, a person has the right to a hearing to review their
detention (Part I: Canadian Charter of Rights and Freedoms). Similarly, the Act is
explicit about the right of the formal patient to apply for a hearing to review their
detention and consider cancellation of admission or renewal certificates issued by the
two qualified health professionals. For this reason, review panels accept applications
from formal patients who are detained under the Act.
Three types of review panel applications related to admission and
detention
Classification: Protected A 40
• A formal patient, the patient’s agent, the patient’s guardian, or a person acting on the
patient’s behalf may apply to a review panel to cancel admission certificates or
renewal certificates or for an order for the board to issue a CTO (section 38), using
Form 12 - Application for Review Panel Hearing.
• An automatic review of a formal patient’s admission or renewal certificates occurs at
or soon after 6 months if no review has been applied for earlier (section 39 of the
Act).
• A patient may apply to a review panel to be transferred back to a correctional facility
(section 33), using Form 12 - Application for Review Panel Hearing. If the patient is a
formal patient, the review panel will first need to decide whether to cancel the
admission or renewal certificates.
3.8 Leave of Absence
During hospitalization formal patients may be allowed to spend time outside the facility.
A treatment plan must set out the criteria on which privileges, including leaves of
absence, would be granted (section 9.01(2)(c) of the Act). The treatment plan must be
provided no later than one month after the issuance of a second admission certificate.
A leave of absence
• may be granted based on terms and conditions, such as where patients will be
staying and with whom, for what length of time, and
• requires that patients may still be subject to the supervision and treatment of any
person(s) designated by the board (section 20(2)) of the Act.
Nothing in the Act specifies the length of time for which a leave may be granted; it may
be revoked at any time.
A formal patient detained in or remanded to a facility under the Criminal Code (Canada),
or the Youth Criminal Justice Act (Canada) (formerly the Young Offenders Act) is not
eligible for a leave of absence (section 20(5) of the Act).
Leave of absence decisions and arrangements
The formal patient may request leave, or it may be suggested by the family or treatment
team when a reason arises. These circumstances can include things like being with the
family for a special occasion dinner, cleaning the patient’s apartment or, looking for
employment or a place to live. In practice, a qualified health professional writes an order
for the leave of absence from a designated facility after discussion with the patient,
treatment team, guardian, relevant family, or supportive community members.
The purpose of the leave is usually therapeutic and also gives an opportunity to assess
the patient’s functioning outside of the designated facility. The length of the leave,
medication to be taken and who will be responsible for the patient should be identified.
Classification: Protected A 41
The patient and supervising person, if any, must understand the medication routine and
be aware of the parameters of the leave.
Initial leaves of absence (sometimes called passes) may be quite brief. In the course of
the patient’s hospitalization the duration of leaves may increase as the patient improves
and readiness for discharge approaches.
Absence without leave
Should a formal patient on a leave of absence refuse or neglect to return to a facility,
the facility may declare the patient “absent without leave” and may order a peace officer
to return the patient to the facility by completing a Form 3 - Order to Return a Formal
Patient to a Facility (section 20(4) of the Act).
If a formal patient leaves a facility when a leave of absence has not been granted, the
facility may use Form 3 - Order to Return a Formal Patient to a Facility to order a peace
officer to return the patient to the facility (section 21(1) of the Act). Form 3 - Order to
Return a Formal Patient to a Facility gives peace officers the authority to apprehend and
return the patient to the facility (section 21(2) of the Act).
Information to give a peace officer about the patient named in Form 3
- Order to Return a Formal Patient to a Facility
Peace officers are aided by knowing the physical description of the named patient, any
characteristic mannerisms and identifying marks. They should also be told when the
patient was last seen, what clothes the patient was wearing when last seen and what, if
any, risks the patient poses to self and others when away from the facility.
Staff should notify peace officers if the patient returns voluntarily, or is otherwise
brought back to the facility, so peace officers are aware they need not continue looking
for the patient named in the Form 3 - Order to Return a Formal Patient to a Facility.
3.9 Transfers
There are times when a formal patient may need to be transferred to another healthcare
centre, for example, when required treatment is provided elsewhere or because they
live in another province and are being taken to a facility closer to home. Each situation
where a transfer may occur is outlined in the Act and may require the use of appropriate
forms to maintain the authority of the Mental Health Act certificates in effect at the time.
Formal patients may be transferred
• to another designated facility (section 22(1.1) of the Act),
• to a hospital for treatment, and then returned to the facility (section 23 of the Act),
Classification: Protected A 42
• from outside the province to an Alberta facility using Form 4 - Certificate of Transfer
into Alberta provided that the requirements for an admission certificate are met
(section 24(1) of the Act),
• to a facility outside Alberta if another jurisdiction is responsible for the patient’s care
and treatment, or it is in the patient’s best interests to be cared for in another
jurisdiction, using Form 5 - Transfer of Formal Patient to a Jurisdiction Outside
Alberta (section 25 of the Act).
(For information on signing authority for Forms 4, 5 and 6 see Chapter 3.10, question 5,
in the guide.)
3.10 Discharge
Discharge of a formal patient is most often associated with the end of certification and
detention. There are a number of reasons why certificates may cease to be in effect
(section 31 of the Act).
• When a formal patient no longer meets the certification criteria, the physician must
cancel the admission or renewal certificates (section 31(2) of the Act).
• When a formal patient’s admission or renewal certificates are cancelled or expire,
the patient must be informed that they remain in the facility voluntarily (section 31(3)
of the Act).
- The patient may continue with mental health treatment as a voluntary
inpatient, or if inpatient treatment is not required, the patient may be
discharged.
- A voluntary patient may also be discharged against medical advice.
• When a review panel finds that the patient no longer meets the criteria for admission
certificates or renewal certificates, the patient is informed of the cancellation of
certificates and may elect to be discharged or continue as a voluntary patient.
The physician who cancels admission certificates or renewal certificates due to the
patient no longer meeting the criteria, must complete a cancellation certificate (Form 2.1
– Cancellation of Admission Certificate or Renewal Certificate, section 31(4) of the Act).
Notice of discharge
Upon discharge of formal patients, notification must be provided to the patient and,
where reasonably possible, their
• guardian, if any,
• nearest relative, unless the patient objects on reasonable grounds,
Classification: Protected A 43
• physician or nurse practitioner who treats the patient in their ordinary day-to-day
health care needs, if known (including a discharge summary and recommendations
for treatment).
When applicable in the notice of discharge it must be stated whether the person has a
certificate of incapacity under the Public Trustee Act (section 32(1) of the Act).
Patients eligible for transfer or discharge who refuse or fail to leave the facility are
legally trespassers. Arrangements may be made to transfer such a patient to another
area in the facility, to an approved hospital, or to a nursing home or other
accommodation (section 32(2) and section 32(3) of the Act).
3.11 Questions about Admission and Detention in Practice
1. Two admission certificates are sufficient authority to detain a person “for a
period of 1 month from the date the second admission certificate is issued.”
What is “1 month”?
Section 22(8) of the Interpretation Act answers this question.
22(8) If an enactment contains a reference to a period of time consisting
of a number of months after or before a specified day, the number of
months shall be counted from, but not so as to include, the month in which
the specified day falls, and the period shall be reckoned as being limited
by and including
(a) the day immediately after or before the specified day, according as
the period follows or precedes the specified day, and
(b) the day in the last month so counted having the same calendar number
as the specified day, but if that last month has no day with the same
calendar number, then the last day of that month.
For example, if a second certificate is issued January 5, the patient may be lawfully
detained until the end of the day February 5.
Because section 22(8)(b) of the Interpretation Act can be confusing, caution should be
taken (and legal advice sought if necessary) when calculating the detention period when
a certificate is issued near the end of a month when the next month has fewer days
(e.g., when a second certificate is issued on January 30, but February only has 28 days,
the patient may be lawfully detained until the end of the day on February 28.)
Classification: Protected A 44
2. does the Act give direction regarding the content requirements of the
discharge summary provided to physicians and nurse practitioners and the
timeframe within which this must occur?
Section 32 of the Act states that discharge notices are provided to physicians and nurse
practitioners who treat the patient in their ordinary day-to-day health care needs, if
known, which will include a discharge summary, any recommendations for treatment
and, if applicable, state whether a certificate of incapacity, under the Public Trustee Act,
exists for that patient. (This includes certificates formerly issued under the Dependent
Adults Act that were transferred to the Public Trustee Act in October of 2009.)
The intent of the discharge summary is to keep physicians and nurse practitioners who
treat the patient in their ordinary day-to-day health care needs apprised of sufficient
information and advice about the patient so effective follow-up treatment can be
provided.
There are no specifics noted and no time frame stipulated in the Act. To be of value, the
notification should be done in a timely fashion, or in other words, within a reasonable
time under the circumstances.
3. Notice of discharge must be given to the patient’s nearest relative unless the
patient objects on “reasonable grounds.” Does the Act give direction on what
would be “reasonable grounds”?
There is nothing specific in the Act. In general, the question of whether there are
reasonable grounds involves both subjective and objective considerations. First, the
patient may give reasons for their concerns. Second, consideration is given to whether it
would be reasonable for a person in the patient’s particular circumstances to object. To
assist with this second consideration, is there information that can be ascertained by
observation or through information received about or from the family that indicates that
a reasonable person would refuse to disclose information in the patient’s particular
circumstances. Section 32 of the Act states that the board must give notice of
discharge, and it is likely that the assessment of whether there are reasonable grounds
will be delegated to a qualified health professional.
4. When is a Memorandum of Transfer to Another Facility – Form 6 required?
Section 22(1) of the Act and Form 6 - Memorandum of Transfer to Another Facility
relate to the transfer from one facility to another; AHS zoning is irrelevant. A Form 6 -
Memorandum of Transfer is required when a patient is being transferred from a
designated AHS facility to either the Grey Nuns Community Hospital, Misericordia
Community Hospital or Villa Caritas, or when the Grey Nuns Community Hospital,
Misericordia Community Hospital or Villa Caritas transfer a patient to a designated AHS
facility.
Classification: Protected A 45
Use of a Form 6 is not required in situations where a detained person is transferred
temporarily to a hospital for medical treatment. In these situations, the patient must be
returned to the designated facility at the conclusion of the treatment (see section 23).
5. When a formal patient with a substitute decision-maker (“SDM”) is transferred
to another designated facility is it necessary to obtain a new consent to
treatment from the SDM or is the SDM’s original consent (as obtained by the
referring facility) still valid?
The Act does not speak to this question. Healthcare providers should follow the consent
policy applicable to their facility. Generally speaking, it may be good practice to obtain a
new consent since consent to treatment is usually specific as to who is providing
treatment. Further, if any new treatment is to be provided, new consent should be
obtained.
6. What signatures are required on Forms 4, 5 and 6?
Form 4 - Certificate of Transfer into Alberta and Form 5 - Transfer of Formal Patient to a
Jurisdiction Outside Alberta require the signature of the Minister of Health or designate.
In Ministerial Order #614/2021, the Minister delegated the powers under sections 24
and 25 of the Mental Health Act to “the person who occupies the position of the senior
official in charge of patient services at each facility as defined in the Mental Health Act
with respect to persons transferred in and out of the facility at which the person holds
the position.”
Form 6 - Memorandum of Transfer to Another Facility requires the signature of the
representative of the board of the sending facility.
Healthcare providers requiring information or confirmation of names of those with
appropriate signing authority should contact a senior administrative person in their
service (e.g., Director or Executive Director for Addiction and Mental Health Services).
7. Can Protective or Security Services in an emergency department access the
patient’s mental health forms (e.g., admission certificates) to confirm the
“validity” of the certificate(s) and/or their role in detaining the patient if
required?
Traditionally, the role of protective services/security services has not included reading
certificates to verify information documented by clinicians. In practice, it is the
responsibility of the treatment team to supply accurate, timely, “need-to-know”
information that protective services/security services require in order to perform their
duties when the situation warrants their involvement. Such information might include a
patient’s certification status, possible elopement risk, or risk of harm to self or others.
With this information the security team can minimize and manage risks to self, the
Classification: Protected A 46
patient, staff, and the public in the performance of their role. Security personnel can rely
on the information given to them by healthcare professionals (such as the fact that a
patient is certified) without checking the certificates.
Notwithstanding the above, regardless of whether protective services/security services
are facility/regional health authority employees or contracted to provide services, they
are “affiliates” under the Health Information Act; therefore, they can access and use
patient’s health information in a manner consistent with their duties to the
facility/regional health authority. However, the Health Information Act mandates that
they should only access and use the minimum amount of health information necessary
to carry out their purpose.
8. What mechanism is used to record cancellation of certificates?
The physician who cancels a formal patient’s admission certificates or renewal
certificates must complete a cancellation certificate (Form 2.1 - Cancellation of
Admission Certificates or Renewal Certificates, section 31(4) of the Act). Form 2.1 -
Cancellation of Admission Certificates or Renewal Certificates requires the physician to
document the reasons for the cancellation of the certificate based on the facts observed
by the physician, and the facts communicated by others.
A Form 2.1 is not required when admission certificates or renewal certificates expire, or
when a review panel cancels admission certificates or renewal certificates. As well,
section 9.1(3) of the Act states that admission certificates or renewal certificates are
cancelled on the issuance of a CTO. A Form 2.1 is not required in those situations.
9. Can a formal patient be charged with a criminal offence that allegedly
occurred while they had formal status?
Yes. All persons in designated facilities, including formal patients, are subject to the
Criminal Code (Canada). Should an alleged offence be committed by a formal patient
while in a facility (e.g., the assault of another patient or a staff member), healthcare
providers (or others) can notify their local police service to lodge a complaint.
10. When a formal inpatient is charged with a criminal offence that allegedly
occurred while they had formal status, where will they be detained?
Where a formal inpatient will be detained depends upon the nature of the charge. For
instance, if a formal patient is charged with a non-detainable offence (a criminal
offence that the criminal justice system deems most appropriately dealt with by a Notice
to Appear in Court), the person receives a Notice to Appear in Court and remains an
inpatient under the care of the clinical team at the designated facility. (In practice, the
patient may be transferred to a unit other than the one where the offence occurred.)
Classification: Protected A 47
In a circumstance where the formal patient has assaulted someone on an inpatient unit
of a designated facility and is charged with a detainable offence (a criminal offence
that the criminal justice system deems suitable to result in incarceration), the person
may not be released by the judge pending trial but, since a formal patient cannot be
incarcerated in a remand facility or jail, must be returned to the designated facility. In
such a situation the attending physician may be of the opinion that the person is
unsuitable for continued care at the facility where the offence occurred. The physician
may give their written opinion and request of the judge (if the Court has not already
ordered it), that the formal patient be moved to a designated forensic facility or unit for
treatment in a more secure setting.
The formal patient’s transfer is authorized by the Court and coordinated by the police
and the treatment teams at both designated facilities. All current Mental Health Act
certificates (or copies thereof, depending on the facility’s policy) and required legal
papers such as the Detention Order must accompany the formal patient to the
designated forensic facility. Local policies/procedures developed for such a contingency
will facilitate the transfer of care of the formal patient from a designated facility to a
forensic designated facility.
11. Are a formal patient’s Mental Health Act certificates still valid when a facility
has a photocopy of the certificate instead of an original?
Yes, the certificate is still valid. However, the original certificate may be required by a
review panel or Court during a hearing.
For the patient to be able to understand the reason for their detention and for the review
panel, legibility of the certificate is a primary concern. In order to provide a fair hearing,
the panel must be able to read the reasons for the issuance of any certificate. As
examples
• “based on the following facts, observed by me, and/or communicated to me by
others” are written by physician(s) on a certificate of mental incompetence to make
treatment decisions,
• “the facts observed by me and/or communicated to me by others” provide reasons
for a patient’s detention under admission/renewal certificates,
12. “the facts on which I formed the above opinion” support the issuance of a community
treatment order. Is an original signature required on all Mental Health Act
forms?
An original signature is required on each Mental Health Act form that is deemed
appropriate to the situation. Without an original signature, there can be practical
problems and/or evidentiary problems during a review panel hearing.
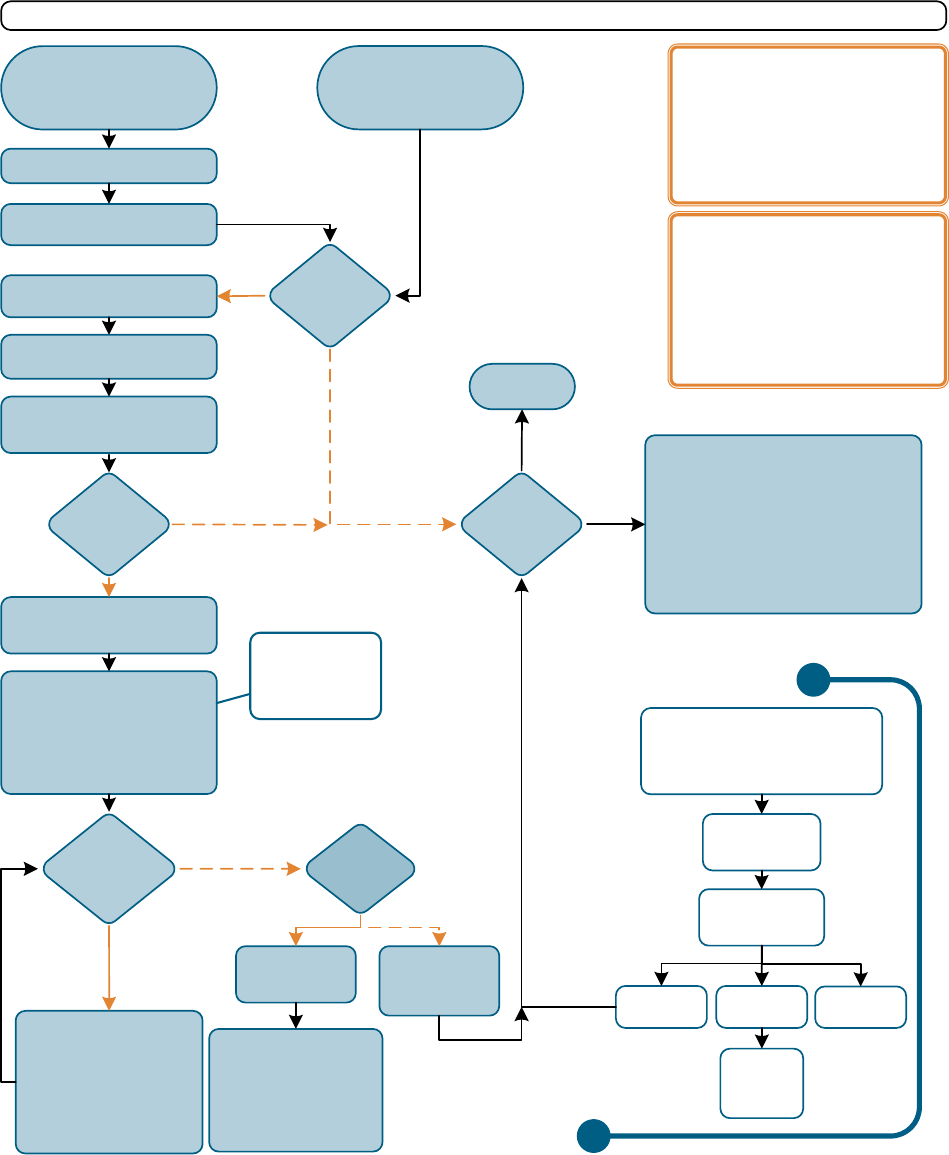
Classification: Protected A 48
3.12 Flowchart: Formal Patient
Refer to the Mental Health Act and its regulations for more comprehensive information. Reliance on this document is solely at th e user’s risk; AHS is not responsible for errors or omissions and will not be respons ible or liable for any
claims arising based on the use (or misuse) of information contained herein. Th is material may be repro duced or copied in full for edu catio nal and program dev elo pment purpo ses or not-fo r-prof it or no n-commercial activities without
permission. © 2022 Alberta Health Services
Person apprehended under
Statement of Peace Officer on
Apprehension (Form 10)
or Warrant (Form 8) (A)
Person
meets ALL 4
criteria?
(B)
QHP issues 2nd Form 1 within 24
hours of arrival at DF or issuance
of 1st Form 1 (C)
YES
YES
NO
Person conveyed to
DF or
SL
QHP performs examination as
soon as possible at
DF or
SL
Consider:
•
admission as voluntary patient
•
discharge with treatment
recommendations & community
resources
•
consulting legal counsel
•
CTO options
For persons with impaired capacity,
consider options under AGTA or PDA ( H)
to identify the SDM
QHP on staff at DF examines
person within 24 hours of arrival
at DF or issuance of 1st Form 1
Patient
continues to
meet admission
criteria
(F)
Renewals: 2 QHPs (at least
1 psychiatrist & 1
DF
staff)
complete separate exams &
issue renewal certificates
(Form 2)
1st renewal: 1 month
2nd renewal: 1 month
All subsequent: 6 months
Review panel
hearing within
21 days (F)
Form 12 submitted to review panel to:
•
challenge admission/renewal
certificates or
•
request a
CTO (G)
Review panel
issues decision
QHP issues 1st Admi ssion
Certificate (Form 1)
(C)
Certificates
cancelled
If person NOT at a DF, convey
within 72 hours to DF
See Key Points for Reference Details A-I (over)
Oc to ber 202 2
Certificates
maintained
CTO ordered
Certificates
maintained
until CTO
issued
Has a CTO
been issued?
Formal patient
status ends (F)
Physician issues
Form 2.1
(unless Forms 1
or 2 have expired)
QHP examines person through
course of normal duties
OR
Person may:
•
remain voluntarily
•
be discharged to
community
•
have additional treatment
needs/recommendations
not contained in CTO
Discharge
NO
Person is now formal patient
DF responsible to:
•
notify patient & others of formal
status (expires at 1 month) and
rights under MHA ( D)
•
ensure Form 1's have been
reviewed for completeness
(E)
NO
NO
YES
YES
NO
YES
Person
meets ALL 4
criteria?
(B)
LEGEND
QHP - Qualifie d Hea lth Pro fessional
DF - Designated Facility
SL - Secure Lo cation
CTO - Community Tr eatment Order
AGTA - Adu lt Guardian & Trustee Act
PDA - Personal Directives Act
SDM - Substitute Decision Maker
MHPA - Mental Health Pa tient Advocate
NOTES
•
If patient p resents vo luntarily
•
Patient or oth ers may access MHPA a ny time
after 1st Form 1
•
If after 6 months of being a for mal patient and a
review panel hea ring has n ot bee n requeste d,
one will be automatically scheduled
•
See (I) for con trol pro visions
Further
treatment
required?
Applying for review
panel hearing
An application can be
made for a re view
panel hearing at any
point while person is a
formal pati ent (G)
Classification: Protected A 49
Definition of Mental Disorder
(MHA s.1(1)(g))
A substantial disorder of thought, mood,
perception, orientation, or memory that grossly
impairs: judgment, behavior, capacity to
recognize reality or ability to meet the ordinary
demands of life, but does not include a disorder in
which the resulting impairment is persistent and is
caused solely by acquired or congenital
irreversible brain injury.
A. Apprehension by Warrant or Peace
Officers Statement
(MHA s.10/12)
To apprehend a person who requires examination,
Judge or Peace Officer have grounds to believe:
I.
A person is suffering from mental disorder AND
within a reasonable time, likely to cause harm
to others or to suffer negative effects, including
substantial mental or physical deterioration or
serious physical impairment, related to the
mental disorder – OR
II.
A person is not complying with their CTO.
Judge’s Warrant: (Form 8)
•
Anyone can submit a Form 7 to a judge at a
provincial court with sworn information (see
above: A.I. or A.II.)
•
Only used if examination cannot be arranged
through any other means.
Peace Officer’s Power: (Form 10)
•
Used if proceeding under a judges warrant
would be dangerous.
B. Formal Patient Certification Criteria
(MHA s.2)
1)
Suffering from a mental disorder
2)
Potential to benefit from treatment for the
mental disorder
3)
Within a reasonable time, likely to cause harm
to others or to suffer substantial mental or
physical deterioration or serious physical
impairment, related to the mental disorder
4)
Unsuitable for admission to DF other than as a
formal patient
C. Admission/Renewal Certificates
(MHA s.4/7/8)
Gives the authority to care for, observe, examine,
assess, treat, detain & control the person.
Effect of One Admission Certificate
•
Apprehend (if required) & convey person to DF
(if not there already) w/in 72 hours of issuance.
•
Valid up to 24 hours from person’s arrival at DF
if conveyed under authority of MHA, or from
issuance of first Form 1 if presented voluntarily.
Effect of Two Admission Certificates
•
Valid up to 1 month from date of second
admission certificate.
Renewal Certificates
•
Must be issued within 24 hours after exam.
•
Both renewal certificates must be completed
prior to expiry of existing certificates.
Formal Patient Key Points
Mental Health Act (MHA) of Alberta
Refer to the Mental Health Act and its regulations for more comprehensive information. Reliance on this document is solely at the user’s risk; AHS is not responsible for errors or omissions and will not be
responsible or liable for any claims arising based on the use (or misuse) of information contained herein. This material may be reproduced or copied in full for educational and program development purposes
or not-for-profit or non-commercial activities without permission. © 2022 Alberta Health Services
All Mental Health Act forms can be found on the website: https://www.albertahealthservices.ca/info/Page1256.aspx
For additional information on the Mental Health Act please visit https://www.albertahealthservices.ca/info/mha.aspx
For any enquiries about these materials please email: MHAandCTO.Enquiries@ahs.ca
D. Notifying Patients & Others
(MHA s.14(1))
Who to notify:
•
Formal patient (i) (ii)
•
Guardian* (if any) (i) (ii)
•
Nearest relative* (unless patient objects on
reasonable grounds) (i) (ii)
•
One person designated by patient (if any) (ii)
* Reasonable efforts must be
made to inform these people
What to include in the notification:
i: Using simple language, and an interpreter if
required, review reason for certificate issuance,
patient’s right to apply to a review panel and
patient right to have legal representation
ii: Provide:
•
copies of admission/renewal certificates,
•
summary of assessment of competency to
make treatment decisions
•
written statement with the following
requirements:
reason for issuance, authority & duration
right to apply for a review panel hearing to
appeal certificates, or to request a CTO be
ordered
function & contact information of the review
panels
patient’s right to legal counsel & steps to
obtain free legal services
function & ways to contact the MHPA
patient’s right to free & timely access to
patient records relevant to review panel or
Court of King
’s Bench hearing
E. Completeness Review
(MHA s.8.1)
Admission & renewal certificates must be
reviewed to ensure all fields are completed. The
process for meeting this requirement, including
who is responsible, may vary by zone.
F. Additional Notification Considerations
•
Notifying patient and others must be completed
upon initial admission AND each subsequent
renewal (see D).
•
A written treatment plan is required to be
provided to patient 1 month after admission as
a formal patient. See section 9.01.
•
Notice of discharge must be given to patient’s
guardian, if any, and nearest relative (unless
patient objects on reasonable grounds).
•
A discharge summary with treatment
recommendations should be provided to the
patient’s regular health care providers.
G. Review Panels
(MHA s.14 & 34-43)
•
Composed of a chair or vice-chair (lawyers), a
psychiatrist & a member of the public.
•
The formal patient, or anyone on their behalf,
may apply for a hearing via Form 12 to:
cancel admission/renewal certificates
request a CTO
overturn a physician
’s certificate of
incompetence to make treatment decisions
•
The formal patient has the right to legal
representation at all review panel hearings
•
Prior to a hearing, formal patient is entitled to
free & timely access to patient records relevant
to review panel.
•
A board or attending physician may apply to
review panel for a treatment order.
•
Any decision or order of the review panel may
be appealed to the Court of King’s Bench.
H. Mental Capacity & Decision Making
All adults are presumption of competent.
Admission as a formal patient does not change
this presumption. If a patient is assessed to lack
capacity, consider options under AGTA: https://
www.alberta.ca/adult-guardianship.aspx
If a personal directive is in place, consider
enacting it though a Schedule 2 or 3 form. See
https://www.alberta.ca/personal-directive.aspx
The MHA addresses competency rather than
capacity (s.26-27). See Competency & Consent
for Formal Patient Flowchart for additional
information.
I. Control Provisions
(MHA s.30)
The MHA authorizes minimal use of reasonable
force, by mechanical means or medication –
without patient consent
– as necessary to prevent
serious bodily harm to the person or another.
Means used must have regard for the physical
and mental condition of the person.
Additional Information
•
In addition to the prescribed MHA forms
referenced, all providers are expected to follow
professional standards and organizational
guidelines for documentation.
•
Formal Patient Certificates (admission/renewal)
are cancelled on the issuance of a CTO (MHA
s.9.1(3)).
•
For additional information on CTO’s:
Community Treatment Order – Issuance or
Renewal Flowchart
•
Terms used in this documents are specific to
the MHA. For definitions, see MHA s.1.
#Form Name Completed by NOTES:
1 Admission Certificate 2 QHP 1 must be a physician and member of the staff of the facility
2 Renewal Certificate 2 QHP 1 must be a psychiatrist
2.1 Cancellation of Admission Certificate or Renewal Certificate Physician
8 Warrant Judge
10 Statement of Peace Officer on Apprehension Peace Officer
12 Application for Review Panel Hearing Formal Patient / SDM / QHP / Other
October 2022
Classification: Protected A 50
CHAPTER 4: Rights of Formal and Voluntary
Patients
This chapter will cover
• what rights are extended to adults and minors who are formal patients,
• how and when formal patients are notified of their rights,
• how formal patients can apply to a review panel to cancel their admission or
renewal certificates, or for an order for the board to issue a community treatment
order (CTO),
• how the Mental Health Patient Advocate (Patient Advocate) promotes and
protects the rights of patients under one or two certificates,
• what rights are extended to both formal and voluntary patients,
• how formal patients have the right to consent to and refuse treatment (though the
right may be limited in specified circumstances), and
• questions about formal and voluntary patients’ rights in practice.
In the Constitution Act, 1982, the Canadian Charter of Rights and Freedoms
(Charter) outlines a number of rights that are guaranteed to all, including the right
to life, liberty, and security of the person. Mental health legislation in Alberta and
other Canadian provinces provides for involuntary detention and treatment in
defined circumstances. The legislation creates a number of “checks and
balances” to protect individuals, such as specialized review panels to hear
applications relating to involuntary detention and treatment.
The meaning of “the board” in the Act
When the Mental Health Act imposes a duty on or grants a power to the “board”, in
practice this is likely delegated to employees or physicians within the facility, depending
on the circumstances. Readers are encouraged to check with management in the
facility to determine to whom a particular responsibility or power has been delegated.
When formal patients are notified of their rights
When one admission certificate is issued, the individual named on the certificate
is advised that they are being held under the Act and for how long. An individual
detained under one certificate is also advised of the right to counsel as this is a
Charter right. The individual will be given contact information for the Patient
Advocate. Neither the right to contact the Patient Advocate, nor the right to
counsel, following the issuance of one admission certificate are governed by the
Act, but both are important (in addition to advising of the reasons for detention). It
Classification: Protected A 51
is not until two admission or two renewal certificates are issued that a
person is deemed a formal patient and can be detained involuntarily at a
designated facility beyond 24 hours.
4.1 Notification of Certification and Right to Hearing before
Review Panel
When two admission or renewal certificates are issued, section 14 of the Act
obliges the board of the facility to notify specific individuals of the certification and
the reasons for certification. In clinical practice, this responsibility has been
delegated to facility staff or physicians (e.g., reviewing the contents of the
certificate with the individual at the time the patient is given their copy).
Simple language is used to inform:
1) the formal patient, 2) the patient’s guardian and, unless the patient objects on
reasonable grounds, 3) the patient’s nearest relative, of the following
• the reason the admission certificates or renewal certificates were issued and,
• the patient’s right to apply to the review panel to cancel the admission or renewal
certificates, or for an order for the board to issue a CTO, and
• the patient’s right to legal counsel.
A written statement must also be given, and may be given to as many
as four people:
1) the formal patient, 2) the patient’s guardian, 3) one person designated by the patient
and, unless the patient objects on reasonable grounds, 4) the patient’s nearest relative.
In summary, this written information must include (section 14(1) of the Act)
• the reason, in simple language, for the issuance of the admission or renewal
certificate,
• the authority for the patient’s detention and the length of the detention,
• the function of review panels,
• the right to apply to the review panel for cancellation of the admission or renewal
certificates, or for an order for the board to issue a CTO,
• the name and address of the chair of the review panel assigned to the facility where
the patient is located,
• the patient’s right to legal counsel,
• the steps for the patient to follow to obtain free legal services,
Classification: Protected A 52
• the function of the Patient Advocate,
• the patient’s right to contact the Patient Advocate, and the mechanisms for making
that contact, and
• the patient’s right to obtain free and timely access to the patient’s medical records
relevant to a hearing before a review panel or the Court of King’s Bench.
The board must also provide 1) the formal patient, 2) the patient’s guardian, 3) one
person designated by the patient and, unless the patient objects on reasonable
grounds, 4) the patient’s nearest relative with copies of the admission certificates or
renewal certificates, and a summary of the assessment made of the patient’s
competence to make treatment decisions.
In the event of language difficulty, a suitable interpreter is to be accessed who can
provide the above information verbally and in writing in the language spoken by the
formal patient or their guardian (section 14(2) of the Act).
If the patient has designated another person to receive notices, the facility is to mail a
copy of all notices and information required to be given to the patient to the person at
the address provided by the patient.
4.2 Notification of the Right to Communication, Visitors, Legal
Counsel, and the Mental Health Patient Advocate
All patients have the right to
• send and receive written communications from outside the facility without the
communications being opened, examined, delayed, or withheld (section 15 of the
Act),
• meet with visitors at approved times, unless a qualified health professional considers
that a visitor would be detrimental to the patient’s health (section 16(1) of the Act),
• visits from legal counsel at any time (section 16(2) of the Act), and
• contact the Patient Advocate for information, advice or to lodge a complaint.
4.3 Right to Treatment and a Treatment Plan
On a patient’s admission, the board of a designated facility must provide the diagnostic
and treatment services that the patient (whether formal or voluntary) is in need of and
that the staff of the facility is capable of providing and able to provide (section 19(1) of
the Act).
Classification: Protected A 53
The board must ensure that a formal patient is provided with a written individualized
treatment plan not later than one month after the issuance of a second admission
certificate (section 9.01(1) of the Act). The treatment plan must set out
• the type of treatment expected to be provided to the formal patient,
• the criteria on which release of the formal patient would be granted, and
• the criteria on which privileges, including leaves of absence, would be granted.
4.4 Right to Consent to or Refuse Treatment
Mentally competent patients generally have the right to consent to or refuse treatment
with some very limited exceptions. If a formal patient is not mentally competent, their
agent, guardian, or nearest relative can consent or refuse to consent to a specific
treatment on the formal patient’s behalf (section 28 of the Act). That treatment should
not be given until consent has been received from the patient or the patient’s SDM. If a
formal patient who is mentally competent or their SDM objects to any treatment the
patient is receiving or will receive, a qualified health professional must not administer
the treatment unless a review panel makes a treatment order (section 29(1) of the Act,
Form 15 – Decision of Review Panel Regarding Treatment).
4.5 Control
Admission certificates and renewal certificates provide the authority to control the
person named in the certificates (sections 4(1), 7(1), 8(3), and 23(2) of the Act). The
authority to “control” is also provided by Forms 4, 8, 10, 23, and the authority also is
shared when the patient is transferred to a hospital for medical treatment (section
23(2)).
Section 30 of the Act stipulates that the authority to control a person under the Act
without the person’s consent is only to the extent necessary to prevent serious bodily
harm to the person or to another person. Control is exercised by the minimal use of
such force, mechanical means, or medication as is reasonable with regard to the
physical and mental condition of that person.
Staff and physicians have a responsibility to ensure safety for the patients
in their care and also have the right to safety in their workplace.
It is important to remember that “control” is different than “treatment”.
Patients have a right to refuse treatment (unless under a treatment order
or a Form 11 with consent from an SDM), but do not have a right to refuse
to be controlled. This distinction may be discussed with patients. If
interventions or medications are used to control behaviour, not treat the

Classification: Protected A 54
patient, staff must document the behaviour requiring control and the
measures used.
4.6 Right of Formal Patients to a Second Opinion Regarding
Competency to Make Treatment Decisions
In situations where an agent or nearest relative has made a treatment decision on
behalf of an incompetent formal patient, and the incompetent formal patient objects to
the treatment, a second opinion must be sought from a physician regarding the patient’s
competency to consent to treatment. (This requirement does not apply when the
patient’s guardian has made a treatment decision.) Treatment cannot be given pursuant
to the consent provided by the agent or nearest relative unless the second physician is
also of the opinion that the patient is not mentally competent to make treatment
decisions (section 28(5) of the Act).
4.7 Right of Formal Patients to Apply to Review Panels
A review panel is a group of three people with knowledge in the application of the
Mental Health Act. When a formal patient applies to a review panel a hearing is held.
There is no cost to the formal patient for the hearing and the decision of the review
panel is made known to the patient immediately or at the most, within 24 hours.
(Chapter 5 of the guide gives a full description of the application process, review panels
and their functions.)
Formal patients have the right to apply to a review panel to request that
• admission certificates or renewal certificates be cancelled, or the board be ordered
to issue a CTO (sections 14(1), 38(1) and 41(1) of the Act). The formal patient’s
agent, guardian, or another person may make this application on the formal patient’s
behalf.
• the physician’s certificate of incompetence to make treatment decisions be cancelled
(sections 27(3) and 41(1)(b) of the Act). The formal patient’s agent or guardian may
make this application on the formal patient’s behalf.
Making an application on another person’s behalf implies:
• The person is aware of the application and supportive of it being made on their behalf
• There is a practical reason the person is not making their own application (e.g., paranoia as
a result of the mental disorder, inability to hold a pen, etc.)
In a hearing, the formal patient and their representative (e.g., the patient’s legal
counsel) have the right to be present during the presentation of any evidence and to
cross-examine any person who presents evidence. The only exception is when the
review panel is of the opinion that disclosure of information to the patient might seriously
Classification: Protected A 55
endanger the safety of another person (section 37(4) of the Act). All proceedings of the
review panel must be conducted in private, and no other person has the right to be
present without the prior consent of the chair of the review panel (section 37(2) of the
Act). Members of the treatment team may be present to provide information at the
review panel hearing, or to provide support to the patient.
4.8 Right to Appeal to Court of King’s Bench
A patient may appeal any decision to the Court of King’s Bench. This would typically
happen if the patient is unsuccessful in challenging admission or renewal certificates or
a certificate of incompetency to make treatment decisions before the review panel. The
appeal is a rehearing of the matter on the merits (section 43(4) of the Act). The appeal
must be commenced within 30 days after the receipt of an order or a written decision of
a review panel (section 43(1) of the Act).
4.9 Questions about Rights of Formal and Voluntary Patients in
Practice
1. What written information is staff obliged to give the formal patient regarding
the review panel?
The Act stipulates that a written copy of the admission or renewal certificates (which
includes the reason and authority for admission and detention and how long the
detention lasts) must be given to the formal patient.
The Act requires that formal patients be given additional information in writing, including
the function of the review panel, the name and address of the review panel chair, the
right to apply to the review panel for cancellation of admission certificates or renewal
certificates or for an order for the board to issue a CTO, as well as a statement the
patient has the right to obtain free and timely access to the patient’s medical records
relevant to a hearing before a review panel.
It is good practice for clinicians to provide formal patients, guardians,
agents, and nearest relatives with fact sheets on formal patients, review
panels and Legal Aid. Alberta Health Services has created the Written
Statement of Certification and Acknowledgment of Notification/Patient
Rights and the Formal Patient Information Sheet to meet these
requirements. These resources, as well as additional written material on
CTOs and the role of the review panel with CTOs are available on Alberta
Health Services Insite and are available for use by Alberta Health Services
and Covenant Health staff.
A. Are there additional Resources available?
The following fact sheets are also available for downloading:
Classification: Protected A 56
1. Mental Health Act Information for formal patients
https://open.alberta.ca/publications/mental-health-act-information-for-
formal-patients
2. Mental Health Act Information about mental health review panels
https://open.alberta.ca/publications/mental-health-act-information-
about-mental-health-review-panels
3. Mental Health Act Information for persons subject to a community
treatment order
https://open.alberta.ca/publications/mental-health-act-information-for-
persons-under-community-treatment-order
B. The Patient Advocate provides brochures Your rights under the Mental Health
Act: One Admission Certificate; and Your rights under the Mental Health Act:
Formal Patient
C. Legal Aid Alberta provides legal services for mental health matters. Their
website is located here: https://www.legalaid.ab.ca/services/mental-health-
law/
D. Mental Health Act forms, including Form 12 - Application for Review Panel
Hearing are available on the AHS website:
https://www.albertahealthservices.ca/info/page1256.aspx
2. How soon after two admission or renewal certificates are issued are formal
patients to be notified of their certification and rights?
It is recommended that formal patients be given such information promptly and without
delay.
3. Why is it important for a formal patient to be notified without delay of their
certification and to receive information about the review panel?
This is important because the person is being detained involuntarily. The Charter rights
of individuals detained in Canada include the right to be notified promptly that they are
being detained, the reasons they are being detained and how they can apply for a
hearing to have their detention reviewed. Under the Act, that review of detention takes
the form of a review panel hearing.
4. What if the patient does not understand their rights when they are notified of
certification?
Classification: Protected A 57
At the time of admission many formal patients are so ill they are unable to comprehend
the information provided. Some patients may have a language difficulty which will
necessitate finding an interpreter.
Staff must document the time(s) they attempted to give notification and what
circumstances, if any, prevented them from doing so. Documenting attempts to deliver
verbal and written notification reflects the healthcare provider’s awareness of
requirements under the Act and the patient’s rights. When formal patients have difficulty
understanding or receiving information about their rights due to the nature of their
illness, staff should repeat their efforts to explain. Successive attempts should be
documented. Staff taking over care of the patient can complete the notification process
when the situation or patient’s condition permits. It is also good practice to document
what information was given, and the patient’s reaction to, as well as, apparent level of
understanding of the information.
Review panels, courts, the patient’s legal representatives and the Patient Advocate may
look for documentation as evidence that the patient was given rights information
promptly, or if applicable, what prevented the patient from receiving complete
information promptly.
Remember, section 14(1) of the Act requires that information also be given to the formal
patient’s guardian, if any, as well as one person designated by the patient and, unless
the patient objects on reasonable grounds, their nearest relative. This helps ensure that
others are aware of the patient’s rights and can advocate on their behalf if necessary.
5. Do formal patients who are minors have the same rights as other formal
patients?
Yes. The Act makes no age-based distinctions regarding rights of formal patients.
Classification: Protected A 58
CHAPTER 5: Mental Health Review Panels
This chapter will cover
• who sits on a review panel and what is its purpose,
• who can apply,
• what applications are heard,
• how legal representatives can access health records,
• how independence and objectivity of review panels are safeguarded,
• how hearings are conducted,
• when review panels may refuse to hold a hearing,
• how review panel decisions can be appealed,
• how formal patients with a guardian under the Adult Guardianship and Trusteeship
Act (AGTA) exercise their rights under the Act, and
• questions about the review panel and hearings in practice.
5.1 Purposes and Composition
Review panels are established to consider applications for a hearing from formal
patients in designated facilities, from individuals subject to a CTO, and also from the
board or attending physician of a formal patient. At the hearings, the review panels
determine whether a formal patient is competent, should continue to be detained
involuntarily in the facility, and/or have treatment decisions made for them. Review
panels also determine whether a person should remain subject to a CTO. Review
panels are composed of three members: a chair or vice chair (who must be a lawyer), a
psychiatrist, and a member of the general public (section 34(4) of the Act). Although the
Act requires the Minister to appoint members of the review panel, the review panel
operates independently from the Minister and the Department of Health when executing
the functions under the Act.
5.2 Types of Applications Heard by a Review Panel
Applications by formal patients, persons who are subject to CTOs, or their
representatives, can be made for the following reasons by completing Form 12 -
Application for Review Panel Hearing:
• objection to treatment (section 29(2) of the Act). The review panel’s decision is noted
on Form 13 - Notice of Hearing Before Review Panel.
• to cancel admission certificates or renewal certificates (section 38(1) of the Act). The
review panel’s decision is noted on Form 17 - Decision of Review Panel Regarding
Admission Certificates, Renewal Certificates or Community Treatment Orders.
Classification: Protected A 59
• to cancel a CTO (section 38(1.1) of the Act). The review panel’s decision is noted on
Form 17 - Decision of Review Panel Regarding Admission Certificates, Renewal
Certificates or Community Treatment Orders.
• to ask for a review of a physician’s opinion that the formal patient is not mentally
competent to make treatment decisions - Form 11 - Certificate of Incompetence to
Make Treatment Decisions (section 27(3) of the Act). The review panel’s decision is
noted on Form 14 - Decision of Review Panel Regarding Mental Incompetence to
Make Treatment Decisions.
• to transfer a person back to a correctional facility (section 33 of the Act). This applies
to persons who have been sent to a facility for psychiatric treatment, after being
sentenced to a correctional facility. If the person is a formal patient, the review panel
will first need to decide whether to cancel the admission or renewal certificates. The
review panel’s decision is noted on Form 16 - Decision of Review Panel Regarding
Transfer Back to a Correctional Facility.
• to order the board of the facility to issue a community treatment order in respect of a
formal patient within a reasonable amount of time (section 38(1) of the Act). The
review panel’s decision is noted on Form 17 - Decision of Review Panel Regarding
Admission Certificates, Renewal Certificates or Community Treatment Orders or
Form 17.1 - Decision of Review Panel Regarding Order for the Board to Issue a
Community Treatment Order.
Applications to review panels from physicians
• Physicians may also apply to a review panel (using Form 12 - Application for Review
Panel Hearing) to order treatment that the physician believes is in the patient’s best
interests (section 29 of the Act) where a mentally competent formal patient refuses
to consent to treatment, or
• where an individual who has legal authority (SDM) to make treatment decisions for
an incompetent formal patient refuses to consent to treatment.
The application process
The patient or the person subject to a CTO has the right to apply to a review panel. In
some circumstances, another person (such as a relative, guardian or agent) may also
apply on their behalf (section 38(1) of the Act). Some applications must be made by the
patient and cannot be made by another person on their behalf (section 27(3) and
section 33(1) of the Act.) When advised that the patient/representative intends to apply
to a review panel, the Act directs the board or qualified health professional to facilitate
the submission of an application (section 14(3)).
Classification: Protected A 60
In practice staff can, for example, answer questions about the patient’s
right to apply to the review panel, provide the patient/representative with
the application (Form 12), answer questions related to completing the
form, confirm the name and address of the review panel chair and help the
patient mail or fax the application to the review panel chair.
The review panel considers the application as soon as it is able to do so and in any
case within 21 days of the chair receiving the application (section 40(4) of the Act)
unless the application is to ask for a review of a physician’s opinion that a formal patient
is not mentally competent to make treatment decisions or for an order directing
treatment to a competent patient who objects. In those circumstances, a hearing must
be held within 7 days of the chair receiving the application (section 40(3) of the Act).
Using Form 13 - Notice of Hearing before Review Panel, the review panel chair replies
to the patient/representative applicant giving written notice of the date, time, and place
of the hearing. The chair of a review panel must give at least 7 days’ notice of the date,
time, place, and purpose of the following of hearings (section 40(1) of the Act):
• to cancel admission certificates or renewal certificates (section 38(1) of the Act)
• to cancel a CTO (section 38(1.1) of the Act)
• to transfer a person back to a correctional facility (section 33 of the Act)
• to order the board of the facility to issue a community treatment order in respect of a
formal patient within a reasonable amount of time (section 38(1) of the Act)
The chair of a review panel must give reasonable notice of the date, time, place, and
purpose of the following hearings (section 40(2) of the Act):
• to ask for a review of a physician’s opinion that the formal patient is not mentally
competent to make treatment decisions (section 27(3) of the Act)
• a physician’s application for a treatment order (section 29 of the Act)
Safeguarding the Rights of the Patient Appearing before a Review
Panel
Information Provided to the Patient
When two admission certificates or two renewal certificates are issued with respect to a
patient, the board is required to provide certain information to the patient as well as
make a reasonable effort to inform the patient’s guardian, if any, and unless the patient
objects on reasonable grounds, the patient’s nearest relative. The information that must
be provided includes the patient’s right to apply to the review panel for cancellation of
the certificates or for an order for the board to issue a CTO, and the patient’s right to
legal counsel. This must be accompanied by a written statement setting out information
Classification: Protected A 61
including the function of review panels, the name and address of the chair, the right to
apply to the review panel for cancellation of the certificates or for an order for the board
to issue a CTO, the patient’s right to legal counsel, and the steps for the patient to follow
to obtain free legal services.
Right to Obtain Free and Timely Access to the Patient’s Medical
Records
The patient has a right to obtain free and timely access to medical records relevant to a
hearing before a review panel (section 14(6) of the Act). The patient does not need to
make a request for medical records.
Confidence that the Hearing will be Fair
The review panel works independently of the facility in which the person is detained. In
addition, the Act contains safeguards to protect the review panel’s objectivity (section 36
of the Act). These safeguards include preventing individuals who previously or currently
have a professional or private relationship with the patient from participating as a review
panel member.
These individuals are those who are
• related by blood or marriage or by virtue of an adult interdependent relationship,
• the patient’s spouse or adult interdependent partner,
• a qualified health professional or other health services provider who is treating or
who has treated the person appearing before the review panel, or
• legal counsel who is acting or who has acted on the patient’s behalf.
Staff of the facility are not permitted to sit as review panel members when the review
panel is considering an application relating to a patient in that facility (section 36(1) of
the Act).
Format of Hearing
The patient must agree to the format for the hearing (section 37(2.1) of the Act). A
review panel may conduct a hearing by any one of the following methods agreed to by
the patient and chair of the review panel: in person, by telephone, by video conference
or any other means of telecommunication.
5.3 Conduct of Hearings
Members of the review panel have all of the powers, duties, and immunities of a
commissioner under the Public Inquiries Act (section 37(1) of the Act).
Classification: Protected A 62
The review panel can
• summon any individuals as witnesses and require them to give evidence and
produce any documents, and
• enforce the attendance of individuals as witnesses and compel them to give
evidence.
Review panel hearings are conducted in private; no person is allowed to attend a
hearing without the permission of the review panel chair (section 37(2) of the Act).
The applicant (e.g., the formal patient or person subject to a CTO) and the applicant’s
representative (e.g., the patient’s legal counsel or agent) have the right to attend when
evidence is presented and to cross-examine any individual who presents evidence
(section 37(3) of the Act).
However, when the review panel is of the opinion that disclosure of information to the
patient might seriously endanger the safety of another person, the review panel may
refuse to disclose information to a patient (section 37(4) of the Act).
5.4 Refusal to Hold a Hearing
Review panels may refuse to consider applications for hearings in limited circumstances
(section 38(4) of the Act). No further application shall be considered by the review panel
if the chair reasonably believes
• the application is frivolous, vexatious, or not made in good faith, or
• there has been no significant change in the circumstances of the formal patient or
person subject to a CTO since the previous hearing.
5.5 Further Function of Review Panels – Deemed Application for
a Hearing
The Act provides for a periodic review of a formal patient’s detention, or a person’s CTO
even if the individual has not applied for a hearing. As a result, a formal patient or a
person subject to a CTO is deemed to have applied to a review panel for a hearing if an
application from the person or representative has not been made to the review panel
within a period of time as set out below.
Formal Patients
Unless an application for review or an order for the board to issue a CTO has been
made (and has not been withdrawn or cancelled) within 6 continuous months of the
admission certificates or renewal certificates being signed, the review panel will conduct
a hearing as if the patient applied for it and consider cancellation of the admission or
Classification: Protected A 63
renewal certificates (section 39(1) of the Act). This is commonly referred to as a ‘6-
month review’.
Regardless of the timelines for the deemed review hearings, a patient can apply for a
review panel hearing at any time.
The Person Subject to a Community Treatment Order
CTOs can be renewed for periods of 6 months and there is no limit on how many times
the CTO may be renewed if the person continues to meet the criteria. The person who
is subject to the CTO is deemed to have applied to the review panel for cancellation of
the CTO on the second renewal and every second renewal thereafter (i.e., every year)
unless an application has been made in the month preceding the renewal (section 39(2)
of the Act).
Regardless of the timelines for the deemed review hearings, a person subject to a CTO
can apply for a review panel hearing at any time.
5.6 Appeal of Review Panel’s Decisions
Any decision of a review panel may be appealed to the Court of King’s Bench.
• There are costs associated with filing the Court of King’s Bench appeal.
• The appeal must be commenced by Originating Notice within 30 days of the receipt
of the review panel’s order or decision (section 43(1) of the Act).
• The appeal is a rehearing of the matter on the merits (section 43(4) of the Act).
• The appeal is heard in private unless the Court directs otherwise (section 43(8) of
the Act).
• The Court may direct that a transcript or minutes taken by a review panel be put into
evidence along with any further evidence the Court considers necessary (section
43(4) of the Act).
• The order of the Court of King’s Bench is final and not subject to appeal (section
43(5) of the Act).
5.7 The Formal Patient who has a Guardian under the Adult
Guardianship and Trusteeship Act (AGTA)
When a person who has a guardian under the AGTA is admitted as a formal patient,
they have the same rights as other formal patients under the Mental Health Act. The
following questions and answers address clinical situations that may arise when the
AGTA and the Mental Health Act intersect in practice.
Classification: Protected A 64
Regarding the Right to Apply for Review of Certification
1. Can a formal patient with a guardian (under the AGTA) apply to a review panel
in order to cancel certification without the guardian’s consent?
Yes, The Act specifies only a small number of reasons why a chair may refuse to hear
an application (see section 38(4)),
• that the application is frivolous, vexatious, or not made in good faith, or
• that there has been no significant change in circumstances since the previous
hearing by the review panel.
Regarding Consent to Release Health Information to Legal Counsel
for the Hearing
2. An adult formal patient with a guardian under the AGTA has applied for a
review panel hearing. Can this patient consent to release of information for the
facility to give the patient’s legal counsel access to their health record for the
purposes of the review panel hearing? Or is the guardian’s consent required?
Provided the guardian has authority over legal matters, the formal patient cannot
consent to the disclosure of their health information to their legal counsel. In these
cases, consent from the patient’s guardian is required.
If the guardian does not have authority over legal matters, then the formal patient can
consent to the disclosure of their health information to their legal counsel.
Written consent from the patient or patient’s guardian, as appropriate, should be
obtained in accordance with the facility’s policies regarding the disclosure of health
information.
Regarding Right to Appeal Physician’s Certificate of Incompetence
3. If a formal patient has a guardian, and a Form 11 - Certificate of Incompetence
to Make Treatment Decisions is issued, is the patient able to make an
application to the review panel and request that the physician’s certificate of
incompetence be cancelled (without the guardian’s consent)?
Yes. Section 27(3) of the Act states that the patient is entitled to have the physician’s
opinion reviewed by a review panel if the patient applies for the review by sending
notice of application to the review panel chair in the prescribed form (Form 12 -
Application for Review Panel Hearing).
Regarding Appeal to the Court of King’s Bench
Classification: Protected A 65
4. Can a formal patient with a guardian (under the AGTA) appeal review panel
decisions to the Court of King’s Bench without the guardian’s consent?
It is up to a Court as to whether they would “hear” an appeal. There is case law
supporting the position that once a guardian has been given the authority to commence
legal proceedings on behalf of a represented adult (as is often granted in guardianship
orders), the patient no longer has this authority. Formal patients should seek advice
from their legal counsel (e.g., Legal Aid) since counterarguments may exist.
5.8 Questions about Review Panels and Hearings in Practice
1. Can a formal patient or person subject to a CTO have an interpreter at the
review panel hearing?
Yes. In order to hold a fair hearing, the patient must be able to understand what is being
said. A review panel and board collaborate to provide this service.
2. How does the formal patient or person subject to a CTO request Legal Aid
assistance?
Formal patients and people on a CTO have the right to speak to legal counsel. Legal
counsel can explain options and give advice. A formal patient can speak to legal
counsel from hospital and legal counsel is able to visit the patient anytime, as long it is
safe to do so.
Legal Aid Alberta offers a free lawyer, called “duty counsel,” to help patients at review
panel hearings. Requests for duty counsel can be made when applying for a review
panel hearing by checking the box to request free legal representation on the Form 12
application. Legal Aid Alberta can also be contacted at 1-866-845-3425 if the patient
has any questions about Legal Aid Alberta's services.
Applications for legal counsel can be made directly to Legal Aid Alberta at the number
above for the purpose of appealing a review panel’s decision to the Court of King’s
Bench.
3. Does the review panel have to give written reasons for their decisions?
In certain circumstances, yes. A decision must be issued within 24 hours of hearing
applications (section 41(2)(b) of the Act). The review panel must give written reasons
for the decision if the review panel decides not to cancel admission or renewal
certificates or a CTO (section 41(4) of the Act). The review panel may choose to give
written reasons in other circumstances, such as refusal to cancel a Form 11 - Certificate
of Incompetence to Make Treatment Decisions.
Classification: Protected A 66
The Act does not specify the content of the written reasons. The common law (judge-
made law) deals with administrative fairness and decision-making, and under it, written
reasons should include:
• a reference to the legislation under which the review panel has the authority to act;
• the issues before the review panel and the main arguments put forth by the parties;
• the finding of facts on which the review panel based the decision; and
• the reasons and rationale for the decision(s) made by the review panel, making a
connection between information presented and the conclusions reached.
4. Do patients need the assistance of legal counsel in order to exercise their
rights before review panels? What assistance is provided by Legal Aid?
Patients do not need the assistance of legal counsel in order to exercise their rights
before a review panel. However, Legal Aid Alberta provides duty counsel to assist
patients because a hearing before a review panel affects a patient’s Charter rights.
Legal Aid Alberta has stated the following:
Legal Aid Alberta can provide duty counsel to those patients who request
their assistance at all review panel hearings in the province; there is no
need to determine the patient’s financial eligibility.
The legal counsel appointed as duty counsel for Legal Aid will, if possible,
see the patient the day before the hearing and will attend at the hearing.
Duty counsel can present the patient’s case before the review panel, pose
questions to anyone providing evidence and present a summation at the
close of the hearing of evidence.
A patient’s legal representative may visit the patient on the unit anytime if
safe to do so. It may be possible for an available duty counsel to provide
some assistance on the day of the hearing for those patients who decide
(at the last minute) they want help. The difficulty is in not being prepared
since counsel would not have had a chance to read the records or talk to
the patient.
5. Can healthcare providers contact legal counsel/Legal Aid for or on behalf of a
formal patient or person subject to a CTO?
Yes, upon a patient’s request and with the patient’s express consent to contact the legal
counsel and disclose information to the legal counsel (such as the patient’s name, the
fact that they are a formal patient or person subject to a CTO who wishes
representation).
Classification: Protected A 67
6. How does legal counsel representing a formal patient obtain access to the
patient’s health record prior to or during the review panel hearing?
Section 14(6) of the Act provides that if a patient applies for a review the board shall,
without charge and as soon as practicable, provide the patient with a copy of the
patient’s medical records in advance of the hearing before the review panel. The patient
would be able to provide legal counsel with a copy of the patient’s health record.
Alternatively, legal counsel representing the patient may obtain written consent from the
patient or patient’s substitute decision-maker for release of health information, in
accordance with the facility’s policies regarding the disclosure of health information.
7. Are patients or legal counsel charged a fee when they request the health
record for review panel hearings?
No; usual permitted fees associated with producing the health record are waived for
patients under the Mental Health Act who request their health information for the
purposes of review panel hearings. Section 14(6) of the Act stipulates that if a formal
patient applies for a review panel hearing or files an appeal to the Court of King’s
Bench, the board must in advance of the hearing, as soon as practicable, and without
charge provide the patient with a copy of the relevant medical records. This section
prevails despite the provisions of the Health Information Act. If there are concerns about
information that will be disclosed under this section, then advice should be sought from
in-house legal services.
8. At a review panel hearing, does the review panel have the right to access the
original health record of a formal patient?
Yes. Section 17(7)(f) of the Act provides for any health information to be disclosed to a
review panel that is to hear an application from the person to whom the health
information relates. (Also see section 37(1) of the Act and section 4 of the Public
Inquiries Act.)
9. What is the role of the patient’s qualified health professional in a review panel
hearing?
The qualified health professional will present their knowledge of the patient based on
history, treatment, and assessment, and to provide observations of the patient’s
mental status, behaviour, risks, changes, improvement, or deterioration since
hospitalization. Although this information will be in the health record as well, the
onus of proof is on the board of the facility in which the patient is detained or on the
qualified health professional who issued, amended, or renewed the CTO (section 42
of the Act). As such, at a review panel hearing the qualified health professional must
Classification: Protected A 68
be prepared to speak to the criteria under the Act and show how the criteria apply in
the particular circumstances before the review panel and should not rely on the
review panel reading and considering the contents of the health record.
10. Do patients need the assistance of legal counsel in order to exercise their
rights before the Court of King’s Bench?
No; patients can represent themselves in appeals to the Court of King’s Bench.
However, Legal Aid services may be available for this purpose. Patients can also hire
private legal counsel.
11. Is there a cost to the patient for the Court of King’s Bench hearing when a
patient is appealing the review panel’s decision?
Court costs: Yes, a fee will have to be paid to the Court when the patient files the
documentation commencing the appeal. For exact fees, individuals should phone the
Court of King’s Bench directly.
Legal counsel costs: The patient can apply to Legal Aid (see next question) or, if a
patient would like private legal counsel, they will have to pay the legal counsel’s fees (as
negotiated between the patient and legal counsel).
12. Does Legal Aid offer representation and/or assistance with costs to a formal
patient requesting assistance with an appeal to Court of King’s Bench?
This answer depends on the specific facts of each case. Appeals to the Court of King’s
Bench must be initiated within 30 days after the receipt of an order or a written decision
of a review panel (section 43(1) of the Act).
A patient who wants to appeal a decision from the review panel to Court of King’s
Bench may apply for Legal Aid representation/assistance by completing a formal
application to Legal Aid. It is strongly recommended to apply as soon as possible
if Legal Aid assistance is required.
Coverage by Legal Aid Alberta for a Court of King’s Bench appeal is decided on
the basis of merit. Determination of merit may require Legal Aid to contact any
previous legal representation at the review panel related to the appeal to the
Court of King’s Bench. Financial evaluation may also preclude Legal Aid from
providing assistance with an appeal to the Court of King’s Bench.
A decision to refuse coverage by Legal Aid can be appealed by the patient. Legal
Aid tries to proceed with that appeal process quickly and they quite often manage
to make a decision on the appeal before the limitation date for filing with court of
King’s Bench.
Classification: Protected A 69
13. Should staff advise AHS Legal Services when a formal patient or person
subject to a CTO has initiated an appeal to the Court of King’s Bench?
Yes. If staff receives filed court documents in relation to appeal or an individual
indicates they have filed an appeal and would like to provide documents to AHS, then
staff should contact AHS Legal Services for assistance.
14. Who is responsible for initiating the “deemed application” under section 39 of
the Act?
Section 39(1) of the Act states that the review panel chair shall cause the review panel
to hear and consider cancellation of the patient’s certificates; however, in practice, the
deemed application for a formal patient is initiated by the unit on which the formal
patient is detained. For this reason, it is helpful if a designated facility has a system for
recording and tracking a formal patient’s admission and renewal certificate dates as well
as the dates of any review panel applications - including those that were withdrawn or
cancelled. Knowing which formal patient is eligible for a deemed application, the unit
can advise the review panel chair in advance of the 6-month date.
Section 39(2) of the Act states that the review panel chair shall cause the review panel
to hear and consider cancellation of the CTO. The person who is subject to the CTO is
deemed to have applied to the review panel for cancellation of the CTO on the second
renewal and every second renewal thereafter unless an application has been made in
the month preceding the renewal (section 39(2) of the Act).
According to section 9(1) of the Community Treatment Order Regulation, the issuing
qualified health professional is responsible for notifying the review panel of approaching
deemed applications. In practice notification to the review panel is provided by either the
CTO coordinator or the CTO administrative support within the zone.
Classification: Protected A 70
CHAPTER 6: Competence, Consent and Treatment
Decisions
This chapter will cover
• why substitute decision-makers are necessary,
• how competence is determined,
• how competence, consent and treatment decisions related to minors and mature
minors,
• what is meant by ‘best interests’ of the patient,
• when second opinions are required,
• when and why a treatment order is issued,
• why formal patients including minors who are formal patients and physicians apply to
a review panel,
• how review panel decisions about treatment orders and competency are appealed,
• questions about competence, consent, and treatment decisions in practice, and
• a review of the Flowchart and Key Points for Formal Patient, Competency and
Consent for Treatment Decisions.
Introduction
Decisions regarding competency to consent to treatment are separate from the
determination of whether a person becomes a formal patient or subject to a community
treatment order (CTO). In other words, a person may meet the criteria for involuntary
detention as a formal patient or issuance of a CTO and still be deemed to have the
mental competency to make treatment decisions. In general, a competent patient or
person subject to a CTO can consent to treatment on their own behalf. Patients are
presumed to be competent until a determination is made that they are not competent to
make treatment decisions.
If a patient is deemed by a physician to be not competent to make treatment decisions,
consent is provided by a substitute decision-maker (SDM). This general rule applies
regardless of whether the patient is a voluntary or formal patient. Similarly, consent to
treatment is provided by the person subject to a CTO, if competent to make treatment
decisions, or their SDM if not.
There is a significant exception to this general rule: a physician may apply to the review
panel to direct that treatment be administered despite a refusal provided by a formal
patient who is competent to make treatment decisions or the SDM of a formal patient
who is incompetent to make treatment decisions.
Classification: Protected A 71
6.1 Competence
The Act identifies a person as mentally competent to make treatment decisions if they
are able to understand the subject-matter relating to the decisions and able to
appreciate the consequences of making or not making the decisions (section 26 of the
Act).
Pursuant to the Act, an assessment of competency involves a two-part test. A person
may be found not competent to make treatment decisions if they do not meet one or
both parts of the test.
Case law is helpful in interpreting the two-part test in section 26 of the Act. In the
leading decision on consent to treatment, Starson v Swayze, [2003] S.C.C. 32, the
Supreme Court of Canada commented on the first part of the test as follows:
The person must be capable of intellectually processing the information as
it applies to his or her treatment, including its potential benefits and
drawbacks. Two types of information would seem to be relevant: first,
information about the proposed treatment; and second, information as to
how that treatment may affect the patient’s particular situation. Information
relevant to the treatment decision includes the person’s symptoms and
how the proposed treatment may affect those symptoms.
The person must have the ability to process, retain and understand information related
to the treatment decision.
The second component of the test is that the person be able to appreciate the
reasonably foreseeable consequences of a decision or lack of decision. In considering
the second part of the test in Starson v Swayze, the Supreme Court of Canada
commented that:
The patient must be able to acknowledge his or her symptoms in order to
be able to understand the information relevant to a treatment decision.
Agreement with a medical professional’s diagnosis per se, or with the
“label” used to characterize the set of symptoms, is not, however,
required.
The second part of the test for capacity will not be met where it is demonstrated that the
person is unable to apply the information about the proposed treatment to their own
circumstances.
The person does not have to actually understand the subject-matter and appreciate the
consequences. The person must have the ability to understand the subject-matter and
apply the relevant information to their circumstances, and be able to weigh the
foreseeable risks and benefits of a decision or lack thereof.
Classification: Protected A 72
Not all formal patients who agree to treatment are competent under the
Act to consent; a physician makes the determination.
6.2 Minors and Mature Minors
Minors
A patient under the age of 18 years is presumed to be a minor patient without capacity.
Section 28 of the Act speaks to where the patient or person is a minor or is not mentally
competent, and how the decision will be made by a person who is apparently mentally
competent, is available and is willing to make the decisions.
If the minor patient is not considered to be a mature minor, their legal representative
may provide informed consent or refuse to provide informed consent to the
treatment/procedure(s) for the minor patient. This is most often their legally identified
parent or guardian.
Mature Minor
There are times when this presumption of a minor not having capacity to consent to
treatment can be rebutted and the minor patient may be able to provide consent, if the
minor patient is assessed and deemed a mature minor. In practice the outcome of the
mature minor assessment shall be documented in the patient’s health record.
Depending on the assessment of a minor, the “mature minor principle” may apply,
allowing the minor to make treatment decisions on their own behalf. The “mature minor
principle” was explained in the Supreme Court of Canada decision, A.C. v. Manitoba
(Director of Child and Family Services), 2009 SCC 30, [2009] 2 S.C.R. 181:
[46] The latitude accorded to adults at common law to decide their own medical
treatment had historically narrowed dramatically when applied to children.
However, the common law has more recently abandoned the assumption that all
minors lack decisional capacity and replaced it with a general recognition that
children are entitled to a degree of decision-making autonomy that is reflective of
their evolving intelligence and understanding. This is known as the common law
“mature minor” doctrine. As the Manitoba Law Reform Commission noted, this
doctrine is “a well-known, well-accepted and workable principle which . . . raise[s]
few difficulties on a day-to-day basis” (Minors’ Consent to Health Care (1995),
Report #91, at p. 33). The doctrine addresses the concern that young people
should not automatically be deprived of the right to make decisions affecting their
medical treatment. It provides instead that the right to make those decisions
varies in accordance with the young person’s level of maturity, with the degree to
which maturity is scrutinized intensifying in accordance with the severity of the
potential consequences of the treatment or of its refusal.
Healthcare providers are encouraged to contact in-house legal counsel or the Canadian
Medical Protective Association, as appropriate, for legal advice in these situations.
Healthcare providers are also encouraged to reference their facility’s policies and
guidelines regarding mature minors.

Classification: Protected A 73
The following questions may be considered when determining whether or not the minor
may be classified as a mature minor and, therefore, competent to make their own
treatment decisions.
This list of considerations is taken from the 2009 Supreme Court of Canada decision
referenced above dealing with mature minors (paragraph 96):
• What is the nature, purpose, and utility of the recommended medical treatment?
What are the risks and benefits?
• Does the adolescent demonstrate the intellectual capacity and sophistication to
understand the information relevant to making the decision and to appreciate the
potential consequences?
• Is there reason to believe that the adolescent’s views are stable and a true reflection
of their core values and beliefs?
• What is the potential impact of the adolescent’s lifestyle, family relationships and
broader social affiliations on their ability to exercise independent judgment?
• Are there any existing emotional or psychiatric vulnerabilities?
• Does the adolescent’s illness or condition have an impact on their decision-making
ability?
• Is there any relevant information from adults who know the adolescent, like teachers
or doctors?
The preceding list of considerations is not exhaustive; healthcare providers are
encouraged to contact their organization’s internal legal services (e.g., AHS Legal
Services) to obtain a more comprehensive list of considerations.
6.3 Consent
Healthcare providers should follow their facility’s or organization’s policy regarding
obtaining consent from a patient or their SDM.
6.4 Certificate of Incompetence to Make Treatment Decisions
The Act describes all the activities to be completed before treatment can begin for a
formal patient who is considered not mentally competent to make treatment decisions.
Each provision for treatment is balanced by the patient’s right to apply for review, of the
physician’s determination of their mental incompetence to make treatment decisions, to
appeal the review panel’s decision and, in some cases, to object to treatment decisions.
Classification: Protected A 74
Issuance of a Certificate of Incompetence to Make Treatment
Decisions
Section 27 of the Act provides that a physician who believes a formal patient is not
mentally competent to make treatment decisions must prepare a certificate of
incompetence to make treatment decisions (Form 11 - Certificate of Incompetence to
Make Treatment Decisions).
The Form 11 - Certificate of Incompetence to Make Treatment Decisions (sometimes
called a physician’s certificate)
• includes written reasons for the opinion that the patient is not mentally competent to
make treatment decisions,
• must be provided to the formal patient, their agent, guardian, if any, and (unless the
patient objects on reasonable grounds) the patient’s nearest relative, and
• notifies the formal patient that they have the right to have the physician’s opinion
about their competence reviewed by a review panel by sending a Form 12 -
Application for Review Panel Hearing to the review panel chair.
Choosing a substitute decision-maker
After issuing the certificate of incompetence the physician must identify someone under
section 28 of the Act who can make treatment decisions on behalf of the incompetent
formal patient.
See Chapter 7.4 for more information related to consent and competency for persons
subject to a CTO.
6.5 Treatment Decisions Made by a Substitute Decision-Maker
Section 28 of the Act sets out how treatment decisions may be made on behalf of
• minors who are formal patients,
• minors who are subject to a CTO,
• adult formal patients who are not competent to make their own treatment decisions,
and
• persons subject to a CTO who are not competent to make their own treatment
decisions.
These treatment decisions may be made by an individual who is apparently mentally
competent to make treatment decisions, available, willing to make the decisions and is
• the agent of the formal patient or person who is subject to a CTO,
• a guardian of the formal patient or person who is subject to a CTO,
Classification: Protected A 75
• the nearest relative (as defined in the Act) in the case where the formal patient or
person subject to a CTO does not have an agent or guardian, or the agent or
guardian is not available or willing or cannot be contacted after every reasonable
effort has been made, or
• if a formal patient or a person subject to a CTO does not have an available agent,
guardian or nearest relative, the Public Guardian.
Requirements of the substitute decision-maker (SDM)
In order to act as the SDM, who is not the guardian or public guardian, the individual
must
• have been in personal contact with the formal patient or person subject to a CTO in
the past 12 months,
• be willing to assume responsibility for making treatment decisions, and
• make a statement in writing certifying their relationship to the formal patient or
person subject to a CTO, and the facts that establish that they meet the above
requirements (section 28(2) of the Act).
Best interests for treatment decisions
Treatment decisions being made by the SDM, who are not the guardian or public
guardian, must be made in accordance with the best interests of the formal patient or
person subject to the CTO. In determining the best interests, the following
considerations apply under section 28(4) of the Act:
• the patient or person’s mental condition will be or is likely to be improved by
treatment,
• the patient or person’s condition will deteriorate or is likely to deteriorate without
treatment,
• the anticipated benefit from treatment outweighs the risk of harm,
• the treatment is the least restrictive and least intrusive that meets the requirements
above.
A SDM will consider all four and may still make a different treatment decision than the
treating physician. The board is not able to disqualify a SDM to find one that is more
amenable. Instead, if warranted, a section 29 treatment order may be issued.
In practice, an SDM may refuse to make or consent to a treatment decision. This might
be based, for example, on a patient’s previously voiced objection about a treatment that
is being considered or the SDM’s belief that the treatment is not in the best interests of
the patient. The SDM might also refuse to make the decision rather than risk
compromising their relationship with the patient.
Classification: Protected A 76
6.6 Challenging the Certificate of Incompetence by Applying to a
Review Panel
If the formal patient makes an application to a review panel for a review of a Form 11 -
Certificate of Incompetence to Make Treatment Decisions, neither the physician nor the
board can act on the physician’s opinion regarding mental competence pending the
outcome of the application (section 27(4) of the Act). This means if a patient objected to
a treatment, that treatment cannot happen until after a review panel has issued a
decision on a section 27 application. However, treatment consented to by the patient
may continue.
Reasonable notice of the time, date, place, and purpose of the review panel hearing
must be given by the chair of the review panel to specified individuals (section 40(2) of
the Act, and Form 13 - Notice of Hearing Before Review Panel).
A hearing must be held and the decision made and communicated to the patient and
their guardian (if applicable) within 7 days of when the review panel chair receives the
application challenging Form 11 - Certificate of Incompetence to Make Treatment
Decisions (section 40(3) of the Act, and Form 14 - Decision of Review Panel Regarding
Mental Incompetence to Make Treatment Decisions).
There is a presumption at common law that adults are competent to make treatment
decisions. If the physician’s opinion is that the person does not have competence to
make treatment decisions and the formal patient disagrees with this opinion, the onus is
on the board of the facility in which the formal patient is detained to prove that the
physician’s opinion regarding mental competence to make treatment decisions is
correct (section 42(b) of the Act).
If the review panel refuses to cancel the physician’s certificate of incompetence (Form
11 - Certificate of Incompetence to Make Treatment Decisions), the formal patient has a
right of appeal to the Court of King’s Bench (section 43(1) of the Act). The application
for an appeal must be made within 30 days of the decision.
6.7 Second Opinion Regarding Competency when the Formal
Patient Objects to Treatment
Some, but not all formal patients who are not mentally competent to make treatment
decisions can object to the treatment decisions of a SDM and obtain a second opinion
regarding their competency. Section 28(5) of the Act requires a second opinion when
the SDM is the patient’s agent or nearest relative and the formal patient objects to the
treatment. This step does not apply when the SDM is the patient’s guardian or the
Public Guardian.
Classification: Protected A 77
Treatment cannot be given pursuant to the consent provided by the SDM who is an
agent or nearest relative unless the second physician is also of the opinion that the
patient is not mentally competent to make treatment decisions (section 28(5) of the Act).
To recap, if a formal patient states that they do not want the treatment consented to by
a SDM who is an agent or nearest relative, the physician must get a second physician’s
opinion regarding whether or not the patient is mentally competent to make treatment
decisions.
If the patient objects to the treatment decision of a guardian or Public Guardian, under
the Act a second opinion is not required.
6.8 Reasons to Apply to a Review Panel for a Treatment Order
The board or a physician may apply to a review panel using Form 12 - Application for
Review Panel Hearing for a treatment order in three circumstances:
• when the physician is unable to treat a competent formal patient because the patient
will not consent to treatment and the board or physician believes treatment to be in
the best interests of the patient, an application can be made to the review panel for
an order directing that treatment be administered (section 29(2) of the Act),
• similarly, if the SDM refuses consent to treatment on behalf of the formal patient who
is a minor or is not mentally competent to make treatment decisions, the board or
physician can apply to the review panel for a treatment order (section 29(2) of the
Act), or
• if a second physician does not agree that the patient is incompetent to make their
own treatment decisions in cases where the SDM is an agent or nearest relative and
the patient has objected to the treatment.
If a competent formal patient or a formal patient’s SDM (under section 28 of the Act)
objects to any existing or proposed treatment, that treatment cannot be provided
unless a review panel makes a treatment order under section 29(1) of the Act.
Response to review panel hearing application
Reasonable notice of the time, date, place, and purpose of the review panel hearing
must be given to the applicant, the patient, the patient’s agent, or guardian, one person
designated by the patient, and, unless the patient objects, the patient’s nearest relative
(section 40(2) of the Act, and Form 13 - Notice of Hearing Before Review Panel).
Within 7 days of when the review panel chair receives the application, a hearing must
be held and the decision made and communicated to the patient and their agent or
guardian (if applicable) (section 40(3) of the Act).
Classification: Protected A 78
6.9 Best Interests Considerations in Treatment Orders
At the review panel hearing, the physician provides evidence and reasons why they are
applying for a treatment order. Before making an order that treatment be administered,
the review panel must be satisfied that (under section 29(3) of the Act)
• the attending physician has examined the formal patient,
• the proposed treatment is in the best interests of the formal patient with regard to the
following considerations
- the patient’s mental condition will be or is likely to be improved by treatment,
- the patient’s condition will deteriorate or is likely to deteriorate without
treatment,
- the anticipated benefits from treatment outweigh the risks of harm,
- the treatment is the least restrictive and least intrusive treatment that meets
the above requirements.
“Note: this is the only type of review panel hearing where a patient’s best interests may
be considered by the panel in making their decision”
6.10 Second Opinion of Treatment – Best Interests
In addition to hearing evidence provided by the physician and reviewing factors
considered in the best interests of the patient, the review panel may also authorize a
psychiatrist who is not a member of the facility’s medical staff to provide an opinion on
whether the proposed treatment is in the formal patient’s best interests (section 29(4) of
the Act).
Decision by the review panel
• The review panel may either refuse to make a treatment order or make an order
directing that treatment be administered.
• The treatment order may be subject to any conditions that the review panel
considers appropriate (section 41(1)(c) of the Act).
• The review panel’s decision is communicated on Form 15 - Decision of Review
Panel Regarding Treatment with the date and notice that the decision can be
appealed to the Court of King’s Bench within 30 days after receipt of the decision.
Court of King’s Bench Appeal
Appeals can be made in two circumstances.
• The patient has the right of appeal to the Court of King’s Bench within 30 days after
receipt of the decision (section 43(1) of the Act). This would normally happen if a
review panel makes an order directing that treatment be administered.
Classification: Protected A 79
• Similarly, if a review panel refuses to direct that treatment be administered, the
physician who applied for the treatment order has a right of appeal to the Court of
King’s Bench.
Provision for treatment while the patient is appealing a treatment
order issued by a review panel to the Court of King’s Bench
• The Act is silent on whether a formal patient can be treated in these circumstances.
However, there is case law supporting the position that treatment can
proceed/continue after the review panel has issued a section 29 treatment order
while the patient is appealing to the Court (until the Court renders a decision).
• A patient may, however, apply to the Court for a “stay” to prevent/stop treatment until
the Court has heard the appeal.
If the treatment order is upheld by the Court of King’s Bench, no further appeals are
possible.
6.11 Psychosurgery
Psychosurgery can never be performed on a formal patient unless the patient consents,
and the review panel orders that the surgery may be performed (section 29(5) of the
Act).
Meaning of “psychosurgery”
“Psychosurgery” means any procedure that, by direct or indirect access to the brain,
removes, destroys, or interrupts the continuity of histologically normal brain tissue, or
that inserts indwelling electrodes for pulsed electric stimulation for the purpose of
altering behavior or treating psychiatric illness. ”Psychosurgery“ does not include
neurological procedures used to diagnose or treat intractable physical pain or epilepsy
where those conditions are clearly demonstrable (section 1(1)(m) of the Act).
Electroconvulsive therapy (ECT) is not considered psychosurgery.
6.12 Questions about Consent, Competency and Treatment
Decisions in Practice
1. When a formal patient has a guardian is it necessary to assess the patient’s
competence to consent to treatment or is it automatically the role of the
guardian to be the SDM?
The Act does not address whether the formal patient’s competence has to be assessed
when the formal patient has a guardian. It simply says “a physician who is of the opinion
…”
Classification: Protected A 80
Section 27 of the Act states that if a physician is of the opinion that a formal patient is
not mentally competent to make treatment decisions, the physician shall complete and
file Form 11 - Certificate of Incompetence to Make Treatment Decisions. Section 27(3)
of the Act anticipates that a copy of the form will be given to the formal patient’s
guardian (among others), thus it is reasonable to interpret that the legislature intended
Form 11 - Certificate of Incompetence to Make Treatment Decisions to be filled out
even when a formal patient has a guardian.
Section 28 of the Act provides that the formal patient’s guardian can be the incompetent
formal patient’s decision-maker for treatment decisions. Thus, if the issuance of Form
11 - Certificate of Incompetence to Make Treatment Decisions is not challenged under
section 27 of the Act, then the guardian automatically has decision-making authority.
2. Where in the Act does it specifically state that treatment cannot be provided
without the patient’s informed consent?
The common law (judge-made law) deals with requirements relating to consent to
treatment. Case law has established that treatment without consent may be negligence
or battery. As such, informed consent to treatment must be sought from patients or their
SDMs.
This is reflected in section 29(1) of the Act which provides that “If a formal patient who is
mentally competent to make treatment decisions or a person referred to in section 28(1)
objects to any treatment the patient is receiving or will receive at a facility, a qualified
health professional shall not administer the treatment unless the review panel makes an
order under this section.”
There are exceptions: A review panel may order treatment under section 29 of the Act
despite a formal patient’s or SDM’s refusal. Also, when the treatment is “emergency
treatment” it can proceed without consent (so long as there are no known previously
expressed wishes to the contrary).
3. If a formal patient is mentally incompetent to make treatment decisions and
objects to the treatment decisions made by an SDM when is a second
physician’s opinion required?
Section 28(5) of the Act requires this second opinion only when the SDM is the patient’s
agent or nearest relative; this step does not apply when the SDM is the patient’s
guardian or the Public Guardian.
4. Can the guardian of a formal minor patient sign them out of hospital against
medical advice?
No. When a person is made a formal patient under the Act, no matter the age, the
certificates are sufficient authority to detain the person in the designated facility until the
Classification: Protected A 81
certificates are cancelled by a physician, review panel, Court of King’s Bench or they
expire (section 7(1) of the Act).
The guardian should be encouraged to discuss with the physician their concerns and
reasons for wanting discharge of the minor who is a formal patient. If there is no
satisfactory resolution, they can make an application to the review panel to cancel
certificates (assuming an application to a review panel has not already been made) or
contact legal counsel or the Patient Advocate.
5. How are mental health treatment decisions made on behalf of minors who are
formal patients?
Section 28 of the Act deals with treatment decisions made on behalf of formal patients
who are under the age of 18 and sets out a list of SDMs. That list should be consulted in
order to determine the appropriate SDM.
Notwithstanding section 28 of the Act, it may be possible to argue that a “mature minor”
who is a formal patient can make their own mental health treatment decisions.
Healthcare providers should contact their in-house legal counsel or the Canadian
Medical Protective Association, as appropriate, for legal advice in those circumstances.
6. How are mental health treatment decisions made on behalf of minors who are
voluntary patients in a designated facility?
Section 28 of the Act only deals with treatment decisions made on behalf of minors who
are formal patients or are subject to CTOs.
In practice, the majority of minors coming to hospital for psychiatric care are brought in
by guardians who make treatment decisions on the minor’s behalf even if the patient is
voluntary and is in agreement with the admission and treatment.
7. Can a Substitute Decision Maker (SDM) under the Act be from outside of
Alberta?
The legislation does not mandate that the agent, guardian or nearest relative be from
Alberta. In choosing an SDM, section 28 of the Act sets out an order of precedence for
selecting the SDM and directs that the person be apparently mentally competent,
available, and willing to make the decision, etc.
If an incompetent formal patient’s nearest relative (e.g., the patient’s spouse)
meets the criteria for an SDM but declines to be the SDM, is the next choice for
SDM the son or daughter or the Public Guardian?
The next choice in this scenario would be the ‘son or daughter’ pursuant to section
1(1)(i)(i)(B) of the Act. The Public Guardian is only the substitute decision-maker where
Classification: Protected A 82
there is no agent, guardian or ‘nearest relative’ (as that term is defined in section 1(1)(i)
of the Act).
8. If a formal patient or person subject to a CTO has expressed wishes while
competent, do those wishes have to be taken into account by their agent or
nearest relative when making treatment decisions on the patient’s behalf?
“Expressed wishes” are not addressed in the Act; in Alberta, the agent or nearest
relative must make decisions in the formal patient’s (or person subject to a CTO) best
interests and is not bound by the Act to the patient’s prior expressed wishes. Best
interests’ criteria are set out in section 28(4) of the Act.
However, there may be a conflict where a patient has written clear instructions in their
personal directive since section 14 of the Personal Directives Act provides that the
agent must follow the patient’s clear instructions. In that instance, legal advice should
be obtained.
9. How does the Mental Health Act work with the Alberta Guardianship and
Trusteeship Act (AGTA) with regards to an adult who lacks capacity and is a
formal patient (e.g., non-emergent treatment)?
If a mental health treatment decision is needed for an adult who lacks capacity to
make treatment decisions and is a formal patient, look to section 28 of the Act, which
allows such decisions to be made by the patient’s agent (under a personal directive),
guardian (as per Court Order granted under the former Dependent Adults Act or under
the AGTA), or nearest relative.
• If the formal patient does not have a guardian or agent, or the agent or guardian is
not available or willing to make the decision or cannot be contacted after every
reasonable effort has been made, then the formal patient’s nearest relative (as
defined in the Act) can make the decision.
• If there is no one to make the decision after looking at all of the foregoing, then the
Public Guardian can make the decision.
• Co-decision-making orders, supported decision-making, or specific decision-makers,
as outlined in the AGTA, are irrelevant in this situation and should not be looked to
with respect to mental health treatment for adults who lack capacity, who are formal
patients or who are subject to a CTO.
If a treatment decision relating to the patient’s physical health is needed for an adult
who lacks capacity to make treatment decisions and is a formal patient, look to the
AGTA and the Personal Directives Act as to whom can consent to such treatment.
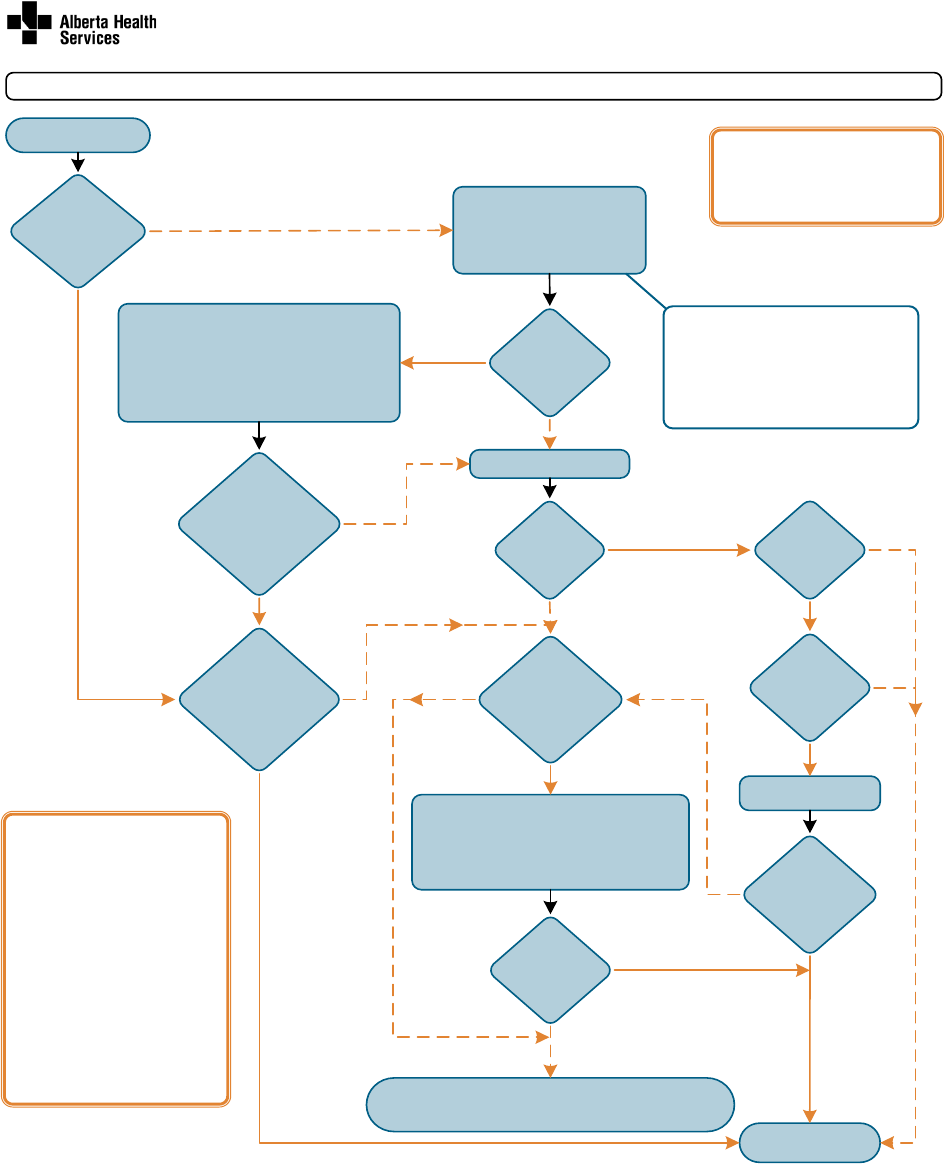
Classification: Protected A 83
6.13 Flowchart: Competency & Consent – Formal Patient
NO
Refe r to the M en ta l He alth Act a nd its r egul at ions for mor e compr eh ensi ve i n for mati on . Reli an ce o n this d ocume nt i s sole ly at the use r’s risk; AHS is not responsible for errors or omissions and will not be responsible
or lia ble fo r an y cla ims ar isin g ba sed on the use (or mi suse ) of i nform ati on co nt ai ne d he rein. Th is mate ria l may be r ep ro du ced o r cop ied in full for e du cati ona l an d pr ogra m de velop m ent p urpo ses or n ot -for-profit o r
no n-com mer ci al a ctivit ies wi tho ut per mi ssio n. © 20 22 Alb er ta Health Se rvi ce s
Person is a formal
patient (A)
Competent to
make treatment
decisions?
(B)
Review of
incompetence
requested via
Form 12?
(E)
Patient
consents to
treatment?
SDM
agrees to
treatment?
Treatment
given
Physician completes certificate
of incompetence (Form 11)
(C)
Give notification & copies to
patient and others
(D)
SDM is
patient’s agent
OR nearest
relative?
(C)
Treatment
order
issued?
Patient
objects to
treatment?
(C)
2nd physician
agrees patient is
incompetent?
(C)
Review panel
decides person is
competent to
make treatment
decisions?
(E)
Review panel hearing within 7 days
Until decision made by review panel:
•
no treatment without patient/SDM consent
•
interventions to control patient to prevent
serious bodily harm are permitted (F)
Physician
applies to review
panel for treatment
order
(E)
2nd physician
examines patient
•
No treatment without patient/SDM consent
•
Use of “control” only to prevent serious bodily harm (F)
YE S
YE S
YE S
YE S
NO
NO
Review panel hearing within 7 days.
Until decision made by review panel:
•
the physician
’s opinion of incompetence
may not be acted upon
•
interventions to control patient to prevent
serious bodily harm are permitted (F)
SDM identified (B)
NOTES
•
An application can be made for
a review panel hearing at any
point while person is a formal
patient
•
Review panel decisions may be
appealed to the Court of King’s
Bench anytime within 30 days of
receiving the review panel’s
written decision.
A decision or order of a
review panel MAY be acted
upon, unless a contradictory
order is issued by the Court
of King’s Bench
•
Formal patients may access the
MHPA services at any time
NO
YE S
YE S
NO
NO
NO
NO
YE S
YE S
See Key Points for Reference Details A-F (over)
YE S
Octo be r 20 22
YE S
NO
Competency & Consent - Formal Patient Flowchart
Mental Health Act (MHA) of Alberta
LEGEND
DF - Designated Facility
SDM - Substitute Decision Maker
MHPA - Mental Health Pa tient Advocate
NO
Form 11 is required anytime a
Physician is of the opinion a formal
patient lacks competence to make
treatment decisions including
• Minors (unless assessed as a mature
minor) (C)
• Adults with a guardian or agent

Classification: Protected A 84
Definition of Mental Disorder
(MHA s.1(1)(g))
A substantial disorder of thought, mood,
perception, orientation, or memory that grossly
impairs: judgment, behavior, capacity to recognize
reality or ability to meet the ordinary demands of
life, but does not include a disorder in which the
resulting impairment is persistent and is caused
solely by an acquired or congenital irreversible
brain injury.
A. Formal Patient
(MHA s.1(e), s.2)
A patient detained in a designated facility
pursuant to 2 admission or 2 renewal
certificates. In both cases the following criteria
must be met in the opinion of 2 QHPs:
1) suffering from a mental disorder
2) has the potential to benefit from treatment for
the mental disorder
3) is within a reasonable time likely to cause
harm to the person or others or to suffer
substantial mental or physical deterioration or
serious physical impairment, as a result of or
related to the mental disorder
4)
unsuitable for admission to a facility other
than as a formal patient
B. Mental Competency
(see MHA s.26-28)
Competency means that the person is able to
understand the subject matter relating to, and
consequences of making treatment decisions or
giving consent and the consequences of not doing
so.
When a physician determines a formal patient is
incompetent to make treatment decisions, these
decisions may be made by the:
a. agent of the formal patient (under an
enacted personal directive)
b. guardian of the formal patient
c. nearest relative as defined in section 1(i), or
d. Public Guardian (last resort)
The nearest relative option is not utilized when an
agent or guardian is in place. The SDM shall make
the treatment decisions in the best interest of the
formal patient.
Competency & Consent
- Formal Patient Key Points
Mental Health Act (MHA) of Alberta
Refer to the Mental Health Act and its regulations for more comprehensive information. Reliance on this document is solely at t he u ser’s risk; AHS is not responsible for errors or omissions and will not be
responsible or liable for any claims arising based on the use (or misuse) of information contained herein. This material may be reproduced or copied in full for educational and program development purposes
or not-for-profit or non-commercial activities without permission. © 2022 Alberta Health Services
All Mental Health Act forms can be found on the website: https://www.albertahealthservices.ca/info/Page1256.aspx
For additional information on the Mental Health Act please visit https://www.albertahealthservices.ca/info/mha.aspx
For any enquiries about these materials please email:
MHAandCTO.Enquiries@ahs.ca
C. Incompetence to Make Treatment
Decisions
(MHA s.27, s. 28)
•
When a physician is of the opinion that a formal
patient is not mentally competent to make
treatment decisions, the physician shall submit
a Form 11.
•
Reasons for the opinion that the formal patient
is not mentally competent must be included.
•
When the SDM
is a guardian, any objection from the
patient does not lead to any further
requirements; treatment may proceed on
the guardian's consent.
is an agent or nearest relative, and the
patient objects to treatment, the MHA
requires a second physician examination
and opinion on the patient’s competence,
before treatment can proceed.
•
When a second physician opinion is required,
they would complete a separate Form 11.
•
A mature minor is a person < 18 years old,
who has been assessed and determined as
having the intelligence and maturity to
appreciate the nature, risks, benefits,
consequences, and alternatives of the
proposed treatment/procedure(s), including the
ethical, emotional, and physical aspects.
D. Notifying Patients & Others
(MHA s.27(3))
Who to notify:
•
Formal patient
•
Agent (if any)
•
Guardian (if any)
•
Nearest relative (unless patient objects on
reasonable grounds)
What to include in the notification:
•
A copy of the Certificate of Incompetence to
Make treatment Decisions (Form 11)
•
Written notice that the patient is entitled to
have the physician’s opinion of incompetence
reviewed by a review panel
•
A review panel hearing can be requested by
sending a Application for Review Panel
Hearing (Form 12)
E. Review Panels
(MHA s.34-43, s. 14(1)(b)(x))
•
Composed of a chair or vice-chair (lawyers), a
psychiatrist and a member of the public
•
The formal patient, or anyone on their behalf,
may apply for a hearing via Form 12 to:
cancel admission/renewal certificates
request a CTO
overturn a physician
’s certificate of
incompetence to make treatment decisions
•
The formal patient has the right to legal
representation at all review panel hearings.
•
Prior to a hearing, formal patient is entitled to
free & timely access to patient records relevant
to review panel.
•
A board or attending physician may apply to
review panel for a treatment order.
•
If an application is made to a review panel to
review a physician
’s opinion that a formal
patient is not mentally competent to make
treatment decisions, neither a physician nor the
board shall act on the opinion pending the
outcome of the application.
•
Any decision or order of the review panel may
be appealed to the Court of King’s Bench by
the “applicant” of formal patient.
•
A decision or order of a review panel MAY be
acted upon, unless a contradictory order is
issued by the Court of King’s Bench.
F. Control (MHA s.30)
The MHA authorizes minimal use of reasonable
force, by mechanical means or medication
–
without patient consent – as necessary to prevent
serious bodily harm to the person or another.
Means used must have regard for the physical and
mental condition of the person.
Additional Information
•
MHPA services are available at any time for all
formal patients.
•
In addition to the prescribed MHA forms
referenced, all QHPs and any other staff
assisting, are expected to follow professional
standards and organizational guidelines for
documentation
# Form Name Com pleted by
11 Certificate of Incompetence to Make Treatment Decisions Physician
12 Application for Review Panel Hearing Patient (for review of incompetence opinion) Physician or Board (for Treatment Order request)
October 2022
Classification: Protected A 85
CHAPTER 7: Community Treatment Orders (CTO)
This chapter will cover
• why community treatment orders (CTOs) were created,
• what conditions/criteria must be met before a CTO is issued,
• how consent is handled,
• what is the exception to the need for consent, and how treatment and care plans are
developed,
• what information is contained on the CTO,
• how the person who is subject to the CTO and others are notified of the CTO and
rights under the Act,
• how and when the person subject to a CTO can apply to review panel,
• why and when CTOs are renewed, amended, cancelled, or expire,
• what happens if a person fails to comply with the CTO,
• what processes provide for apprehension and conveyance to a facility when a
person is not complying with a CTO,
• questions about CTOs in practice, and
• a review of the Flowchart and Key Points for Community Treatment Orders (CTO).
Background
Community treatment orders (CTOs) are largely dealt with in section 9.1 of the Act,
although there are references elsewhere (e.g., treatment decisions on behalf of the
person subject to a CTO, section 28 of the Act). The Community Treatment Order
Regulation (CTO Regulation) further clarifies the Act in areas such as:
• how examinations can be conducted for the purpose of assessing whether an
individual should be subject to a CTO (section 2 of the CTO Regulation),
• supervision of CTOs (section 3 of the CTO Regulation),
• how treatment or care is provided (section 4 of the CTO Regulation),
• how circumstances are addressed when a person subject to a CTO is non-compliant
(section 6 of the CTO Regulation),
• copies of documents to be provided (section 7 of the CTO Regulation),
• responsibilities of the issuing qualified health professional and the person
responsible for supervising the CTO (section 8 of the CTO Regulation), and
• review by review panel on renewal of CTOs (section 9 of the CTO Regulation).
Classification: Protected A 86
7.1 Introduction to Community Treatment Orders
Community treatment orders were implemented in Alberta in January 2010. CTOs
expand addiction and mental health service options available to patients and healthcare
providers.
CTOs are intended for persons with serious and persistent mental disorders who have
demonstrated that, without community treatment and support, they will experience
recurring relapses and hospitalizations - frequently as formal patients. The purpose of
CTOs is to provide these individuals with the particular treatment and care they require
in the community, thus breaking the cycle of admission-discharge-readmission.
Both adults and minors who are inpatients (whether formal or voluntary) may be
appropriate for a CTO. In fact, readiness for discharge from hospital can be facilitated
by CTO support and supervision. Additionally, CTOs can be initiated with clients in the
community, as long as all of the criteria are met.
In Alberta, a CTO is not court ordered nor are persons subject to a CTO considered
formal patients. When a CTO is issued, a formal patient’s admission or renewal
certificates are automatically cancelled (section 9.1(3) of the Act). In many (but not all)
circumstances, the person, or someone acting on their behalf under section 28 of the
Act, must give consent for a CTO to be issued.
As well, the context and process of issuing a CTO differs from that of writing admission
or renewal certificates under the Act. Certifying a patient occurs fairly quickly in
response to legislative requirements and the immediate, often urgent, need to detain a
patient in a designated facility. Conversely, issuing a CTO may take place over a
number of days or weeks as the various components are considered and arranged
(e.g., care, treatment, consent, signatures).
7.2 Applicability and Criteria for Issuance of a CTO
In practice, the qualified health professional may determine a person
meets the criteria for issuance of a CTO, but undertake treatment planning
and obtain required signatures before examining the person for the
purpose of completing Parts I and II of Form 19 or 20. This practice
reflects the length of time that is required to complete the planning and
signing processes and ensures actual examinations take place within the
preceding 72 hours of the issuance of the CTO.
Section 9.1 of the Act identifies the criteria that must be met when two qualified health
professionals, one of whom must be a psychiatrist, issue a CTO (Form 19 - Issuance of
Community Treatment Order).
Classification: Protected A 87
To be placed on a CTO the qualified health professionals must each believe that the
person is:
1. Suffering from mental disorder,
2. Has one or more of the following apply:
(i) within the immediately preceding 3-year period the person has on 2 or more
occasions, or for a total of at least 30 days,
(A) been a formal patient in a facility,
(B) been in an approved hospital or been lawfully detained in a custodial
institution where there is evidence satisfactory to the 2 qualified health
professionals that, while there, the person would have met the criteria set out in
section 2(a) and (c) at that time or those times, or
(C) both been a formal patient in a facility and been in an approved
hospital or lawfully detained in a custodial institution in the circumstances
described in paragraph (B);
(ii) the person has within the immediately preceding 3-year period been subject
to a community treatment order,
(iii) in the opinion of the 2 qualified health professionals, the person has, while
living in the community, exhibited a pattern of recurrent or repetitive behaviour
that indicates that the person is likely to cause harm to others or to suffer
negative effects, including substantial mental or physical deterioration or serious
physical impairment, as a result of or related to the mental disorder, if the person
does not receive continuing treatment or care while living in the community,
(iv) a review panel has ordered a board to issue the community treatment order
under section 41,
3. The two qualified health professionals after separate examinations within the
preceding 72 hours must both be of the opinion that the person is within a reasonable
time likely to cause harm to others, or to suffer negative effects, including substantial
mental or physical deterioration or serious physical impairment, as a result of or relating
to the mental disorder, if they do not receive continuing treatment or care while living in
the community (section 9.1(1)(c) of the Act).
4. The treatment or care the person requires must exist in the community, be available
to the person and will be provided to the person (section 9.1(1)(d) of the Act).
5. The person must be able to comply with the treatment or care requirements in the
CTO (section 9.1(1)(e) of the Act).
Classification: Protected A 88
6. Finally, the person or their SDM must either be willing to consent to the CTO or the
circumstances must be such that consent is not needed.
Review Panel Order
A review panel may order a board to issue a CTO in respect of a formal patient (section
9.1(1)(b)(iv) and section 41 of the Act). The CTO must be issued in a reasonable
amount of time in accordance with the criteria in section 9.1 of the Act (section 2.1 of
the CTO Regulation). The formal patient’s admission or renewal certificates remain in
effect until the CTO has been issued, or they have been cancelled by a physician, or
expire, whichever happens first.
Examination by video conference
In order to facilitate examinations of persons in the community and rural areas, section
2 of the CTO Regulation explicitly permits remote examinations by way of video
conference, or other appropriate technology, for the purpose of issuing or renewing
CTOs and for examinations related to apprehension orders.
7.3 Competency, Consent to a CTO and Consent to Treatment
Overview
This section will cover
• the person’s competence to consent to treatment,
• Selection of a substitute decision-maker (SDM), if necessary,
• Exceptions to consent — Issuing a CTO without consent,
• Consent to treatment,
• consent to a CTO is separate from consent to treatment,
• signed consent for the issuing or renewal of a CTO, unless relying on an exception.
Competency
Section 26 of the Act states that “a person is mentally competent to make treatment
decisions if the person is able to understand the subject-matter relating to the decisions
and able to appreciate the consequences of making the decisions”.
A person’s competence should be assessed by a physician to determine whether they
are able to consent to the CTO. As a general rule, the person named in the CTO or their
SDM must consent to the CTO being issued. If they are not competent, this fact, as well
as any reasoning for the conclusion regarding capacity, must be documented in the
health record.
Classification: Protected A 89
Selection of a substitute decision-maker (SDM)
If the person who will be subject to the CTO is not competent to consent to the issuance
or renewal of a CTO
• a SDM’s consent must be provided by a person who is competent to make decisions
on the person’s behalf; selection of an SDM must be made in accordance with
sections 28(1) and 28(2) of the Act, and
• a SDM can consent to a CTO on the person’s behalf (in Part V, Form 19 - Issuance
of Community Treatment Order or Form 20 - Renewal of Community Treatment
Order), as well as consent to the person’s treatment provided in accordance with a
CTO (usually through a separate process with the treatment provider).
Exceptions to consent — Issuing a CTO without consent
If the person who will be subject to the CTO, or their SDM if applicable, refuses to
consent to the issuing or renewal of the CTO, the issuing qualified health professionals
will need to determine whether or not to proceed.
A CTO can be issued without consent if the person has, while living in the community,
exhibited a history of not obtaining or continuing with treatment or care that is necessary
to prevent the likelihood of negative effects to the person, including substantial mental
or physical deterioration or serious physical impairment, as a result of or related to the
mental disorder, or harm to others, and a CTO is reasonable in the circumstances and
is less restrictive than detaining the person as a formal patient (section 9.1(1)(f)(ii)).
Consent to treatment
Consent to treatment is separate from consent to a CTO. Regardless of whether the
CTO is issued with or without the person’s consent (as outlined in the “exceptions to
consent” described previously), informed consent to treatment must be obtained before
any treatment is provided.
• Healthcare providers should follow their facility’s or organization’s policy regarding
obtaining consent to treatment.
• When a SDM consents to treatment on behalf of a person subject to a CTO, a
separate/additional consent form is necessary.
Signatures - Part V: Consent
The issuing or renewal of a CTO is not complete without the signing of the consent
portion in Part V of Form 19 - Issuance of Community Treatment Order or Form 20 -
Renewal of Community Treatment Order. There are three options identified, and one of
them must be completed:
• consent by the person subject to a CTO,
Classification: Protected A 90
• consent by a SDM, or
• no consent - the criteria for issuing a CTO without consent are restated and the
issuing qualified health professionals must sign Part V.
7.4 The Process of Treatment and Care Planning
Having established that the person meets the criteria for a CTO, the qualified health
professional works with a treatment team to prepare a proposed plan of treatment and
care and to ascertain that the required supports, treatment, and care exist in the
community, are available, and will be provided to the person.
The treatment and care plan is integral to the issuance of a CTO and is included in
Form 19 - Issuance of Community Treatment Order (Part III). It may state that the
person who is subject to the CTO must take medications listed in the CTO (which may
be adjusted based on clinical need) and attend appointments, accept telephone, or
email contact or home visits, or receive treatment from listed providers or their
designate. Thus, the development of the treatment and care plan should be done
collaboratively, and, at the very least, include
• the issuing qualified health professional,
• the supervising qualified health professional (if this is not the issuing qualified health
professional),
• the remaining treatment team,
• the person subject to the CTO and their substitute decision-maker if there is one,
and
• any other person, group or organization that will provide treatment or care to the
person in the community
Ongoing supervision of the person subject to a CTO can only be provided by a qualified
health professional (section 3 of the CTO Regulation).
Note: because the person who is subject to the CTO must be able to
comply with the requirements in the CTO they should always be involved
in the development of the CTO even if they are not competent to consent
to the issuance / renewal of the CTO.
The qualified health professional issuing the CTO should meet with the patient and their
SDM, where applicable, to review the purpose of the CTO, the conditions it contains
and the treatment and care plan. The meeting provides an opportunity for the person to
communicate their willingness to participate in and follow the requirements of a CTO.
The qualified health professional should also review the person’s rights relative to the
CTO. See section 7.7 below on Rights.
Classification: Protected A 91
7.5 Contents of the CTO
Form 19 - Issuance of Community Treatment Order is used for issuance of CTOs, and
Form 20 - Renewal of Community Treatment Order is used for renewals of CTOs.
Amendments to CTOs are noted on Form 21 - Community Treatment Orders
Amendments to Community Treatment Order. Under section 9.1(2) of the Act, the CTO
must
• identify and be signed by the issuing qualified health professionals,
• note the dates and times when the examinations occurred,
• explain the qualified health professionals’ separate rationales for issuing the CTO,
• identify the treatment or care plan, the individual responsible for supervision, and
any reporting obligations, and
• satisfy any other requirements provided for in the regulations (e.g., section 4 of the
CTO Regulation requires the signature of the person authorizing services to be
provided by regional health authority).
Noting that Forms 19, 20 and 21 include the written statement, which is part of the form
to facilitate compliance with section 14(1.1) of the Act.
Duration of the CTO
A CTO will be in effect for an initial 6 months after the day it is issued and will
automatically expire unless two qualified health professionals (one of whom must be
a psychiatrist) renew it for another 6 months. There is no limit to the number of times a
CTO may be renewed. There are automatic reviews of a CTO built into the legislation
and also opportunities for the person to apply for a hearing to request that their CTO be
cancelled. A person subject to a CTO may apply to a review panel to cancel the CTO,
see Chapter 5).
7.6 Forms and Signatures
It is important that the information written on the CTO is legible. The documents must
fulfill legislative requirements to state the reasons for the issuance of the CTO, and
contain all necessary signatures and dates.
• The names of the person subject to the CTO, qualified health professionals, and
treatment and care providers must be legible.
• The identified treatment, care and accompanying dates must be legible.
• A CTO is a legal document and is evidence of the terms and conditions the person
must follow to comply with the CTO.
Service providers may consider having their manager or supervisor sign
the treatment and care portion of the CTO in case the specific service
providers change due to unavailability for any reason.
Classification: Protected A 92
Signature to be provided by regional health authority representative
If any services are to be provided by a regional health authority (i.e., AHS), that regional
health authority’s representative
• must sign Part III of the CTO before it becomes effective, and
• must sign any amendments to the treatment or care plan before they become
effective (section 4 of the CTO Regulation).
Copies of forms
The issuing qualified health professional must provide a copy of each CTO and any
associated completed forms to the regional health authority (section 7 of the CTO
Regulation). This is in addition to providing copies to the person and their SDM (if
applicable) and the nearest relative unless the person objects on reasonable grounds
as outlined in 7.7 Rights and Notification below.
The regional health authority must then promptly provide copies to:
• the person who is responsible for supervising the community treatment order, if that
person is not the issuing qualified health professional, and
• the person who is responsible for providing the written statement referred to in
section 8, if that person is not the regional health authority.
the nearest relative of a person who is subject to a community treatment order is
prescribed to be a person to whom a written statement and a copy of an issued,
amended, or renewed community treatment order must be given under section 14(1.1)
of the Act, unless the person subject to the order objects on reasonable grounds.
In Practice: the issuing qualified health professional, may not be the qualified health
professional who supervises the CTO in the community. Only a psychiatrist can issue
an expiry/cancellation form. Both may be supported by other staff so that this
responsibility will be met. Exact processes may vary by RHA.
7.7 Rights and Notification
Persons subject to a CTO, whether minors or adults, have certain rights which are
protected under the Act. Section 8 of the CTO Regulation requires the issuing qualified
health professional to prepare and provide a copy of the issued, amended, or renewed
CTO (Form 19 - Issuance of Community Treatment Order or Form 20 - Renewal of
Community Treatment Order or Form 21 - Amendments to Community Treatment
Order) with the following information (section 14(1.1)(a) of the Act):
• the reason for the issuance, amendment, or renewal of the CTO,
• the authority for the issuance, amendment, or renewal of the CTO,
Classification: Protected A 93
• information regarding the function of review panels,
• the name and address of the chair of the appropriate review panel, and
• the right of the person subject to the CTO to apply to the review panel for
cancellation of the CTO.
“This information is set out in the first section of Forms 19, 20 and 21. A complete and
legible form meets these requirements for written notice.”
This notice must be given by the issuing qualified health professional to:
• the person subject to the CTO,
• the person’s SDM, if any,
• any persons providing treatment or care to the person subject to the CTO,
• an individual designated by the person subject to CTO (section 14(4) of the Act), and
• the nearest relative, unless the person subject to the community treatment order
objects on reasonable grounds.
Verbal explanation
It is pertinent to present information on the contents of the CTO to the person subject to
a CTO and/or their SDM. Information, including the function of the review panel and the
Patient Advocate, should also be communicated verbally, and in simple language.
Interpreter
In the event of a language difficulty, a suitable interpreter must be obtained and the
above information must also be provided in the language spoken by the person subject
to the CTO, or their guardian (section 14(2)(b) of the Act).
Mental Health Patient Advocate (Patient Advocate)
The role of the Patient Advocate extends to a person subject to a CTO (section 45 of
the Act). The person should be advised that they may contact the Patient Advocate for
rights information, expression of concerns, and complaints about their rights, care, and
treatment. The Patient Advocate is authorized to investigate and resolve complaints
from or relating to persons who are subject to CTOs (section 45(1.1)(e) of the Act). The
Patient Advocate may contact and advise a person who is subject to a CTO at any time,
regardless of whether a complaint has been received from or relating to a person who is
subject to a CTO (section 45(1.2) of the Act). The Patient Advocate must notify the
qualified health professional who last issued, renewed, or amended a CTO or issued an
apprehension order where a patient complaint relates to that issuing qualified health
professional (section 5(4) of the Mental Health Patient Advocate Regulation).
Classification: Protected A 94
Written material
Information about CTOs, review panels, Legal Aid and the Patient Advocate is available
to be given the person subject to the CTO and their SDM.
The following fact sheets are available for downloading:
• Mental Health Act Information about mental health review panels
https://open.alberta.ca/publications/mental-health-act-information-about-mental-
health-review-panels
• Mental Health Act Information for persons subject to a community treatment
order
https://open.alberta.ca/publications/mental-health-act-information-for-persons-
under-community-treatment-order
The Mental Health Patient Advocate provides brochures titled Your Rights Under the
Mental Health Act: Community Treatment Orders
Legal Aid Alberta - https://www.legalaid.ab.ca/services/mental-health-law/
Mental Health Act forms, including Form 12 - Application for Review Panel Hearing are
available on the Alberta Health Services website:
https://www.albertahealthservices.ca/info/Page1256.aspx
7.8 Application to a Review Panel to Cancel a CTO
An individual subject to a CTO can request cancellation of their CTO by completing
Form 12 - Application for Review Panel Hearing - available online or from their
supervising qualified health professional, case manager or other mental health staff
working with the individual. The completed Form 12 - Application for Review Panel
Hearing is mailed or faxed to the review panel chair (section 38(1.1) of the Act).
It is important that the Form 12 is sent to the correct review panel chair. However, if a
review panel chair receives an application for review of a CTO outside the chair’s
geographic area, the application will immediately be forwarded by the chair to the
appropriate review panel chair (section 9(2) of the CTO Regulation).
Review panel hearings are held in the area in which the person subject to the CTO
resides. In practice, the team working with the applicant may assist the review panel
chair in organizing the hearings to ensure all appropriate parties are engaged and all
necessary clinical information (e.g., CTOs, amendments, current health record
documentation, if any) is available for review panel consideration and decision-making
(section 17(7)(f) of the Act).
The hearing to consider cancellation of a CTO is held within 21 days of the application
being received by a review panel chair. The review panel can cancel or uphold (refuse
Classification: Protected A 95
to cancel) a CTO, but they cannot amend it. A review panel can cancel a CTO if the
criteria for its issuance are no longer met.
If the application is unsuccessful, the person who is subject to the CTO has a right to
appeal the review panel’s decision to the Court of King’s Bench (section 41(3) of the
Act). The appeal must be initiated within 30 days of receiving the decision. (See
Chapter 5 in this guide for further information about review panels.)
Deemed application
A person who is subject to a CTO is deemed to have applied to the review panel for
cancellation of the CTO on the second renewal and every second renewal thereafter
unless an application for cancellation has been made in the month preceding the
renewal (section 39(2) of the Act).
The person subject to the CTO and their SDM, if any, receive at least 7 days’ notice of
the date, time, place, and purpose of the deemed application hearing from the review
panel chair (section 40(1) of the Act).
According to section 9(1) of the CTO Regulation, the issuing qualified health
professional is responsible for notifying the review panel of approaching deemed
applications.
7.9 CTO Renewal, Amendment, Cancellation or Expiry
Renewal
CTOs expire 6 months after the day they are issued unless they are renewed (Form 20
- Renewal of Community Treatment Order) or cancelled (section 9.2 of the Act). A CTO
may be renewed at any time before its expiry for a period of 6 months (section 9.3 of
the Act and Form 22 – Community Treatment Order Cancellation or Expiry). There is no
limit on the number of renewals allowed. The requirements of section 9.1 of the Act
apply to the renewal except for the requirement that the separate examinations by
qualified health professionals must occur within the immediately preceding 72 hours. In
the case of a renewal, the separate examinations by qualified health professionals must
occur within the immediately preceding 7 days (section 9.3(4) of the Act).
Amendments
The regulations set out a procedure for amending conditions of the CTO (section 9.4 of
the Act). Amendments may include changing the treatment and care plan (such as the
service provider) or the supervising qualified health professional. The person subject to
the CTO may request amendments and, generally speaking, conditions can be
amended by an issuing qualified health professional (in communication with the person
subject to the CTO) at any time. However, the onus remains on the issuing qualified
Classification: Protected A 96
health professional to ascertain whether the required treatment or care is available and
will be provided to the person and whether the person has the ability to comply with the
terms of the amended CTO. An issuing qualified health professional amends a CTO
using Form 21 - Community Treatment Orders Amendments to Community Treatment
Order.
Form 19 - Issuance of Community Treatment Order (Part III) and Form 20 - Renewal of
Community Treatment Order (Part III) state that medication may be adjusted where
indicated by clinical need. In practice, if the medication indicated on the CTO is listed by
class (antipsychotic, antidepressant, mood stabilizer, antianxiety, etc.), rather than
specific medication and dosage, an amendment is not required when making
adjustments to dosage or medications within the same class. If the Form 19 or 20 is
written in this way, an amendment (Form 21 - Community Treatment Orders
Amendments to Community Treatment Order) would only be required if the medication
is changed from one class to another.
Cancellation
Section 9.5 of the Act specifies that CTOs may be cancelled at any time by a
psychiatrist using Form 22 - Community Treatment Order Cancellation or Expiry, if
criteria set out in section 9.1(1)(b) to (d) cease to apply.
In a situation where a person subject to a CTO or, if applicable, their SDM, no longer
agrees to the CTO, they may discuss this with the qualified health professional who is
supervising the CTO. A qualified health professional may, as appropriate, amend the
CTO or if the person is refusing to comply with the terms of their CTO despite best
efforts, issue an apprehension for the person. The person also has the option to apply
to the review panel for cancellation of the CTO, and the review panel will either cancel
or refuse to cancel the CTO.
Notice of cancellation or expiry of CTO
When a CTO expires or is cancelled, Form 22 - Community Treatment Order
Cancellation or Expiry must be completed, including recommendations for continued
treatment or care.
• The person subject to the CTO must be advised.
• Notification is given to individuals who were formally notified when the CTO was
issued, as well as the person’s physician or nurse practitioner who treats the person
in their ordinary day-to-day health care needs, if known (section 14(5) of the Act).
Notification is given and Form 22 - Community Treatment Order Cancellation or Expiry
is completed and distributed by a qualified health professional upon cancellation or
expiry of a CTO (section 14(5) of the Act). Section 8(2) of the CTO Regulation provides
Classification: Protected A 97
that the person responsible for giving notice of expiry or cancellation is the person
responsible for the supervision of the CTO. Section 3 of the CTO Regulation stipulates
that a CTO may be supervised only by a qualified health professional.
7.10 Failure to Comply
Reporting requirement
Individuals identified on the CTO as providing treatment or care to persons subject to a
CTO must report any failure of the person to comply with treatment or care under the
CTO to the regional health authority within 24 hours of becoming aware of the failure to
comply (sections 6(1) and (2) of the CTO Regulation). The notice must be provided on
Form 25 - Community Treatment Order Non-compliance Report.
Upon receiving notice of failure to comply with treatment or care (Form 25 - Community
Treatment Order Non-compliance Report), the regional health authority is obligated to
provide copies of the form to the qualified health professional responsible for
supervision of the CTO within 24 hours (section 6(3) of the CTO Regulation).
Consequences of non-compliance with a CTO
If a person subject to a CTO is not in compliance with the treatment or care in the CTO,
an apprehension order may be issued (section 9.6 of the Act, Form 23 - Community
Treatment Order Apprehension Order). The Act requires that, prior to issuing the CTO
apprehension order, a qualified health professional must be satisfied that reasonable
efforts have been taken to inform the person, and if applicable the SDM, that there is
non-compliance and the need for compliance.
The person subject to the CTO must be provided with reasonable assistance to enable
them to comply with the treatment or care in the CTO and be advised of the
consequences of non-compliance which include
• that an order for their apprehension and conveyance to a designated facility for
examination may be issued, and
• the possibility that the outcome of this assessment may include being admitted to a
designated facility and detained as a formal patient.
Only a qualified health professional may complete the CTO apprehension order.
A person cannot be forced to accept treatment or care or comply
with the treatment or care outlined in a CTO. If they are not complying,
the treatment team will follow the steps outlined above – to support and
inform the person, potentially amend the CTO, and advise the person of
the consequences of continued non-compliance. Consequences include
Classification: Protected A 98
having the person taken to a designated facility for examination with a
possible outcome of admission as a formal patient.
7.11 Processes for Apprehension and Conveyance of a Person
not Complying with a CTO
There are three processes whereby a peace officer may apprehend and convey a
person not complying with a CTO to a designated facility for examination.
1. By carrying out a CTO apprehension order (Form 23 - Community Treatment
Order Apprehension Order)
• A CTO apprehension order is completed and signed by a qualified health
professional who, despite efforts to support the person’s compliance with the CTO,
has reasonable grounds to believe the person subject to a CTO has failed to comply
with the CTO.
• The CTO apprehension order gives a peace officer authority to apprehend the
person, which includes the authority to enter premises, use of physical restraint, and
take the person into custody, care for, detain and control the person during
conveyance to a specific facility to be examined (section 9.6(1) of the Act).
• The qualified health professional must indicate on the CTO apprehension order a
specific facility to which the patient must be conveyed.
• The order expires 30 days after being issued (section 9.6(3) of the Act).
2. By carrying out a judge’s warrant (Form 8 - Warrant)
• A judge’s warrant is issued when someone brings information under oath before a
judge about a person subject to a CTO regarding reasonable and probable grounds
to believe the named person is not complying with their CTO (Form 7 - Information).
• If the judge believes that the person is subject to a CTO and is not complying with
their CTO, and an examination cannot be arranged in another way, the judge may
issue a warrant (Form 8 - Warrant).
• The warrant gives peace officers the authority to apprehend and convey the named
individual to a designated facility for examination (section 10(5) of the Act).
• The warrant to apprehend the person expires in 7 days (section 10(7) of the Act). A
peace officer may under oath request a judge to extend the warrant for a further 7
days (section 11 of the Act). Form 9 - Extension of Warrant is used to extend the
warrant.
3. By acting pursuant to section 12(1) of the Act under peace officer
discretion (Form 10 - Statement of Peace Officer on Apprehension)
Classification: Protected A 99
In order to apprehend and convey the person to a designated facility for examination
pursuant to section 12(1) of the Act, the peace officer must have reasonable and
probable grounds to believe
• the person is suffering from a mental disorder,
• the person is subject to a CTO and is not complying with the CTO,
• the person should be examined in the interests of the person’s own safety or the
safety of others, and
• the circumstances are such that to proceed under section 10 (i.e., judge’s warrant)
would be dangerous.
• The apprehension order gives peace officers sufficient authority to care for, observe,
assess, detain, and control the person. (section 12(2) of the Act).
Examination at a designated facility
As soon as practicable and, at the most, within 72 hours of being conveyed to a
designated facility under Form 23 - Community Treatment Order Apprehension Order,
Form 8 - Warrant or Form 10 - Statement of Peace Officer on Apprehension, the person
subject to the CTO must be examined by two qualified health professionals, one of
whom must be a psychiatrist (Form 24 - Community Treatment Order Examination on
Apprehension). Under section 9.6(4) of the Act, the two qualified health professionals
must each decide whether
• the CTO should be cancelled, and the person should be released without being
subject to the CTO,
• the CTO should continue, amended as necessary, or
• the CTO should be cancelled and the person should become a formal patient, with
admission certificates issued.
7.12 Questions about Community Treatment Orders in Practice
1. When a CTO is issued in respect of a formal patient, are their
admission/renewal certificates automatically cancelled or is a Form 2.1 -
Cancellation of Admission Certificate or Renewal Certificate required as well?
Section 9.1(3) of the Act states that “the certificates of admission or renewal for a formal
patient are cancelled on the issuance of a community treatment order”. No Form 2.1 -
Cancellation of Admission Certificate or Renewal Certificate is required.
2. Who can issue, renew, amend, and cancel CTOs?
A qualified health professional may issue, renew, or amend a CTO. Issuances and
renewals of CTOs require two qualifying health professionals, and one must be a
psychiatrist. Only a psychiatrist may cancel a CTO.
Classification: Protected A 100
3. What can be included in the CTO treatment and care plan?
It is up to the issuing qualified health professional to determine what provisions they feel
can validly be part of a CTO. A CTO treatment and care plan will be specific to the
person subject to the CTO, their needs, and goals. This CTO treatment and care plan
could include, for instance, medications, clinical tests, and other aspects of care. As a
legal document, a CTO should not include unattainable stipulations or provisions, or
provisions that, if not met, would not normally necessitate apprehension and
conveyance to a facility by a peace officer.
4. Is it necessary to document information about a CTO on a health record in
addition to completing CTO forms?
The Act does not speak to documentation on the health record, but a prudent clinician
would document on a person’s health record, for example, the reasons for implementing
a CTO, the discussion about consent and treatment planning, why a CTO was
amended, how non-compliance was handled and under what circumstances a CTO was
cancelled. These are just a few examples of documentation that can provide evidence
of a consensual and supportive CTO process.
5. How do you get all of the providers’ signatures on the CTO?
Ideally, the CTO could be signed by all providers at a case conference. This may not be
feasible due to timing or distance: some providers may be in a different community than
where the CTO is being issued and the case conference held.
The use of fax to obtain the required signatures is permissible. It is imperative that the
CTO be legible. If faxing is necessary, it is recommended that the original CTO be faxed
to each provider. Each provider will sign the treatment and care plan and return the
signed document (may be by fax, original to follow by mail) to the issuing qualified
health professional). DO NOT send the fax to one provider, have them sign and fax
back and then “refax” to the next provider. This will result in an illegible document that is
not acceptable to give to the patient or the review panel (if required).
The process described may result in multiple copies of the pages requiring signatures.
This is preferable to having all the necessary signatures on one document that becomes
very difficult to read due to repeated faxing.
6. At what point does the CTO come into effect?
The CTO is considered issued when two qualified health professionals (one of whom is
a psychiatrist) have signed the CTO on Forms 19 or 20 – Parts I and II (Form 19 -
Issuance of Community Treatment Order and Form 20 - Renewal of Community
Treatment Order).
Classification: Protected A 101
For a CTO to be valid, the two qualified health professionals must have each examined
the person (separately) within 72 hours of signing / issuing, the CTO, or within 7 days if
it is a renewal of the CTO (section 9.3(4) of the Act).
• A CTO cannot be issued until it is known that the treatment or care the person
requires exists in the community, is available and will be provided (section 9.1(1)(d)
of the Act).
• It is prudent for Parts I and II to be signed after all of the care providers have signed
the treatment and care plan in Part III, and consent has been obtained from the
person subject to the CTO or their SDM (or signatures have been obtained from
both qualified health professionals if the CTO is being issued without consent).
• A supervising qualified health professional must be identified (if this is not the issuing
qualified health professional).
• It must be determined whether a SDM is required (e.g., if the person is not
competent).
In practical terms, this may mean that at least one qualified health professional will
examine the person more than once. The first time will be to determine whether the
person is suitable to be considered for a CTO. It may take some time - days or even
weeks - to ensure all of the treatments listed on the order are available (e.g., no waiting
lists) can be provided, that all of the providers have been consulted and agree to and
have signed the order. When all of these components are in place, it may be necessary
for the qualified health professional(s) to re-examine the person to ensure the criteria
are met within the required timelines (72 hours for the issuance of the CTO, and 7 days
for renewals).
Parts I through V of the form must be completed legibly, with all necessary signatures
for the CTO to be issued or “in effect”. It is recommended the Written Statement of the
form also be done when the form is issued in order for the entire form to be complete
and to adhere to the requirement for a written statement in section 14(1.1) of the Act.
7. How long is a CTO valid?
A CTO “expires 6 months after the day it was issued” unless it is renewed or cancelled
(section 9.2 of the Act). The key terms here are “months” and “after”. Computation of
time is clarified in section 22(8) of Alberta’s Interpretation Act. Rather than stipulating
the number of days, the use of the term “month” allows for the variation in the length of
each month. Use of the term “after” is understood to mean the next day.
For example, a CTO issued January 5 would expire July 6; a CTO issued August 30,
2020 would expire February 28, 2021. Note that 6 months plus a day would be February
31st; but February 2021 has only 28 days. Because section 22(8) of the Interpretation
Classification: Protected A 102
Act can be confusing, caution should be taken (and legal advice sought if necessary)
when calculating the 6-month period.
The Act states that a CTO may be renewed at any time before its expiry. This means a
renewal must be completed prior to the expiry of the existing order. As this can be done
any time before the expiry of the current CTO, it is advised to begin this process well in
advance, making specifics of the 6-month expiration less of an issue and allowing time
to ensure all of the criteria will be met, including the availability of the treatment and
care.
8. The Act frequently refers to the “issuing qualified health professional” in
reference to CTOs. Is this the qualified health professional who first issued the
original CTO?
Not necessarily. The regulations define the “issuing qualified health professional” as the
qualified health professional who completed Part I of the most recent Form 19 –
Issuance of Community Treatment Order, or Form 20 – Renewal of Community
Treatment Order, or who amended the CTO (Form 21 – Community Treatment Order
Amendments to Community Treatment Order).
9. Who can supervise a CTO?
The CTO must be supervised by a qualified health professional (section 3 of the CTO
Regulation). A CTO may often be initiated by a psychiatrist while the patient is in a
facility as a formal patient. If the psychiatrist is not able to continue as the supervising
qualified health professional, another community psychiatrist, physician, or qualified
health professional (e.g., nurse practitioner) will need to be identified and agree to take
on the supervisory role. This may occur when the patient is hospitalized in a different
location than the community to which they will return upon discharge.
10. Can a peace officer enter a person’s premises in order to apprehend that
person when executing a CTO apprehension order (Form 23 - Community
Treatment Order Apprehension Order)?
Yes. Section 9.6 of the Act by way of Form 23 - Community Treatment Order
Apprehension Order explicitly gives peace officers authority to enter premises to
apprehend individuals named in the form. Specifically, Form 23 states that it authorizes
peace officers to “take reasonable measures, including the entering of premises and the
use of physical restraint, to apprehend the person who is named in this order and to
take the person into custody for the purpose of conveying the person to the facility”.
This same authority does not exist for sections 10 or 12 of the Act.
11. Having conveyed a person identified in a CTO apprehension order or a judge’s
warrant to a designated facility for examination, is a peace officer also
Classification: Protected A 103
required to complete a Form 10 - Statement of Peace Officer on
Apprehension?
No; duplicate forms are not required. Each one of these three processes, whether Form
8 - Warrant (section 10), or Form 23 - Community Treatment Order Apprehension Order
(section 9.6), or Form 10 - Statement of Peace Officer on Apprehension (section 12),
gives a peace officer authority to apprehend and convey a person subject to, and
believed non-compliant with, a CTO to a facility for examination.
12. If an amendment is made to the CTO, does the whole order have to be re-
written on Form 21 - Community Treatment Orders Amendments to
Community Treatment Order, or can just the change be documented?
It is reasonable to interpret that it is only necessary to show the insertions and deletions
(i.e., the changes), rather than reproduce the entire care plan on Form 21 - Community
Treatment Orders Amendments to Community Treatment Order. That being said, it
would be helpful if those filling out Form 21 include a statement that the person must
still follow the treatment and care plan as outlined in the original CTO (Form 19 -
Issuance of Community Treatment Order) or the renewed CTO (Form 20 - Renewal of
Community Treatment Order) unless a particular requirement is expressly changed on
Form 21.
13. What if there is an irregularity or insufficiency with respect to one of the
Forms connected with a CTO?
Depending on the facts, there is the possibility that the form will be invalid.
Mental Health Act forms are legal documents, so it is important that they are filled out
completely and accurately. If information is missing on a form, or added after the form is
signed, it is possible that the form will not be valid. Healthcare providers may address
specific questions to their organization’s internal legal services.
14. How are treatment decisions made on behalf of minors subject to CTOs?
Section 28 of the Act sets out a list of SDMs for minors subject to CTOs. That list should
be consulted to determine the appropriate SDM. Notwithstanding section 28 of the Act,
it may be possible to argue that a “mature minor” who is under a CTO can make their
own mental health treatment decisions. Healthcare providers should contact their in-
house legal counsel or Canadian Medical Protective Association, as appropriate, for
legal advice in those circumstances. For more information specific to mature minors see
Chapter 6.
Classification: Protected A 104
15. Can outside agencies confirm with a regional health authority (i.e., Alberta
Health Services) whether a CTO is in place with respect to a particular patient?
This issue is governed by the Health Information Act (HIA). Whether or not a person is
subject to a CTO is “health information”, and since a regional health authority is a
custodian under the HIA the health authority can only disclose this type of patient
information if
• the patient has consented in accordance with section 34 of the HIA, or
• the disclosure falls within an exception listed in section 35 of the HIA.
Whether or not the disclosure can occur depends on to whom the health authority is
disclosing, and for what purpose. It is recommended that the Information and Privacy
department for AHS or Covenant Health be consulted with respect to disclosure in
particular circumstances, since the answer will depend on the facts of each situation.

Classification: Protected A 105
7.13 Flowchart: Community Treatment Orders
In Practice: Forms 19 and 2 0 a re 6 pa rt forms required for the issuance and renewal of a CTO respective ly. The issuing QHP may de termine a pe rson meets the criteria for a
CTO , but un dertake treatment planning and obtain signature s under parts III and IV before the re quired examinations and completion of pa rts I and II of Form
19/20. Parts V and th e Written Statemen t are usually the final parts to b e comple ted.
Person being considered
for a CTO issuance/renewal
OR a review panel has
ordered a CTO be issued
(A) (B)
Separate exams
by two QHPs
(at least one must
be a psychiatrist)
(A) (B)
Patient
consents to
CTO?
A (f)
Patient is
competent ?
(C)
Able
to comply
with treatment
or care?
A (e)
Treatment /
care available
in community?
A (d)
Person meets
CTO criteria
A (a,b,c)?
SDM
consents?
(C)
Meets criteria
to issue without
consent?
A (f)(ii)
Assess need
for admission to
hospital or
voluntary treatment
options in the
community (I)
CTO issued (Form 19) or
renewed (Form 20):
• patient and others
notified of
CTO and
rights under MHA
(B) (D) (E)
• CTOs may be
amended via Form 21
if needed or cancelled
via Form 22 when any
CTO criteria are no
longer met (F) (G)
Refer to th e M en ta l Health Act a nd its r eg ulat ions for m ore compr eh en sive in formation . R eliance on this d ocu me nt i s sole ly at the user’s risk; AHS is not responsible for errors or omissions and will not be responsible
or lia ble fo r any claims ar isi n g ba sed on th e use (or mi suse ) of i n for mation co nt aine d he re in. Th is mate ria l may be r ep rodu ced o r cop ied in full for e du cational an d pr og ra m de velopment p urpo ses or n ot-fo r-profit o r
no n-com mercial a ctivit ie s witho ut per mission. © 20 22 Alb er ta He alth Se rvice s
See Key Points for Reference Details A-I (ov er)
Meets criteria
to issue without
consent?
A (f)(ii)
NOTES
•
CTO s :
are issued and renewed for
maximu m per iods of 6 mon ths
automatica lly expire unl ess
renewed prior to 6 months
are not limited in numbe r of
renewals provide d criteria continue
to be met
•
Patient (or SDM) may request a review
panel hearing to cancel a C TO at
anytime
•
MHPA service s acce ssible upo n
issuance of a C TO
Review panel
hearing within 21
days?
(H)
CTO cancelled
(G)
Review panel
requested via
Form 12?
(H)
NO
NO
NO
NO
YE S
LEGEND
CTO - Commu nity Tr eatment Order
QHP - Qualifie d Hea lth Pro fessional
SDM - Sub stitute Decision Maker
MHPA - Mental Health Pa tient Advocate
NO
NO
NO NO
YE S
YE SYE SYE S
YE S
YE S
YE S
YE S
YE S
NO NO NO
YE S
Deemed review: an automatic
review panel hearing is
scheduled at the time of the
2nd renewal and every
2nd renewal thereafter
All parts of the CTO
forms must be
completed within:
• 72 hours of 1
st
examination for
Issuance (Form 19)
• 7 days of the 1
st
examination for
Renewal (Form 20)
In practice, these examinations may
take place before or after other parts
of the process have been completed,
within the noted time frames.

Classification: Protected A 106
Definition of Mental Disorder
(MHA s.1(1)(g))
A substantial disorder of thought, mood, perception,
orientation, or memory that grossly impairs: judgment,
behavior, capacity to recognize reality or ability to meet
the ordinary demands of life, but does not include a
disorder in which the resulting impairment is persistent
and is caused solely by an acquired or congenital
irreversible brain injury.
A. Criteria for CTO
(MHA s.9.1(1))
Two QHPs - one MUST be a psychiatrist - may, issue a
CTO with respect to a person if they meet a) through f):
a. person is suffering from a mental disorder, and
b. one or more of the following apply:
i. within the immediate preceding 3-year period the
person has on two or more occasions, or for a
total of at least 30 days,
A. been a formal patient in a facility or
B. been in an approved hospital or been lawfully
detained in a custodial institution where there
is evidence satisfactory to the two QHP that,
while there, the person would have met the
criteria (for a formal patient) at that time or
those times, or
C. both A. and B. above
ii. the person has within the immediately preceding
3-year period been subject to a CTO
iii.
in the opinion of the two QHPs, the person has,
while living in the community, exhibited a pattern
of recurrent or repetitive behavior that indicates
that the person is likely to cause harm to others or
to suffer negative effects, including substantial
mental or physical deterioration or serious physical
impairment, as a result of or related to the mental
disorder, if the person does not receive continuing
treatment or care while living in the community, or
iv. a review panel has ordered a board to issue the
CTO under MHA s.41,
c.
Two QHPs, after separate examinations of the person
within the immediately preceding 72 hours, are both of
the opinion that the person is within a reasonable time,
likely to cause harm to others or to suffer negative
effects, including substantial mental or physical
deterioration or serious physical impairment, as a
result of or rel ated to the mental disorder, if the person
does not receive continuing treatment or care while
living in the community, and
d. treatment or care the person requires exists in the
community, is available to the person, and will be
provided to the person,
and
e.
in the opinion of each QHP, the person is able to
comply with the treatment or care requirements set out
in the CTO, and
f.
either,
i. consent to the issuing of the CTO has been
obtained,
A. from the person, if they are competent, or
B. in accordance with section 28(1), if they are
not competent
or
ii. consent to the issuing of the CTO has NOT been
obtained, but in the opinion of the issuing QHPs,
A. person has, while living in the community,
exhibited a history of not obtaining or
continuing with treatment or care that is
necessary to prevent the likelihood of
negative effects to the person, including
substantial mental or physical deterioration
or serious physical impairment, as a result of
or related to the mental disorder, or of harm
to others, and
B. a CTO is reasonable and would be less
restrictive than retaining the person as a
formal patient.
Community Treatment Order Key Points
Mental Health Act (MHA) of Alberta
Refer to the Mental Health Act and its regulations for more comprehensive information. Reliance on this document is solely at t he user’s risk; AHS is not responsible for errors or omissions and will not be
responsible or liable for any claims arising based on the use (or misuse) of information contained herein. This material may be reproduced or copied in full for educational and program development purposes
or not-for-profit or non-commercial activities without permission. © 2022 Alberta Health Services
All Mental Health Act forms can be found on the website: https://www.albertahealthservices.ca/info/Page1256.aspx
For additional information on the Mental Health Act please visit https://www.albertahealthservices.ca/info/mha.aspx
For any enquiries about these materials please email: MHAandCTO.Enquiries@ahs.ca
B. Issuing/Renewing a CTO
(MHA s.9.1, s. 9.2, s. 9.3; CTO Reg. s. 1-2)
•
Renewal criteria are the same as issuance criteria
(see A) except the allowable time between the first
examination and completion of all parts of the
prescribed form is 7 days instead of 72 hours.
•
“Issuing qualified health professional” means the QHP
who last issued, renewed, or amended a CTO.
•
Examinations for the purposes of issuance or renewal
may be conducted remotely using any means
considered appropriate by the examining QHP,
including, but not limited to, video conference.
•
A CTO is valid for 6 months and can be renewed
anytime before its expiry.
•
Formal patient admission or renewal certificates are
automatically cancelled upon the issuance of a CTO.
C. Mental Competency
(MHA s.26, s. 28)
Competency means that a person is able to understand
the subject matter relating to, and the consequences of,
making treatment decisions or giving consent and the
consequences of not doing so.
When a physician determines a person subject to a CTO
is incompetent to make treatment decisions, these
decisions may be made by the:
a. agent of the person (under an enacted personal
directive)
b. guardian of the person on a CTO
c. nearest relative as defined in section 1(i), or
d. Public Guardian (last resort)
The nearest relative option is not utilized when an agent
or guardian is in place. The SDM shall make the
treatment decisions in the best interest of the person.
D. Form Requirements
(MHA s.9.1(2) CTO Reg. s.4)
Must be written on the correct and most current version of
the form (Form 19 or 20)
•
Identify and be signed by the issuing QHP, a second
examining QHP, the supervising QHP (if different from
issuing QHP) and all treatment providers
•
Contain the dates and location (city/town & facility) of
the examinations, the rationale/ facts from which the
examining QHPs formed their opinions and the
treatment and care to be provided.
if the treatment and care plan requires services
provided by the regional health authority (i.e., AHS), a
person authorized to approve the service must sign the
CTO (e.g., Program Manager).
E. Notification of CTO Issuance,
Amendment and Renewal
(MHA s.14(1.1), s. 14(2), s. 14(4) CTO Reg. s.7, s.8)
Who to notify:
•
Person subject to CTO
•
SDM under MHA s. 28 (if any)(see C above)
•
Issuing QHP
•
Supervising QHP
•
ALL treatment providers named in the CTO
•
Nearest relative (unless patient objects on reasonable
grounds)
•
One person designated by person subject to CTO (if
any)
What to include in the notification:
•
Copies of issued, amended or renewed CTO
•
Written statement (of Forms 19, 20 & 21) with the
following requirements in simple language, using an
interpreter if required :
reason & authority for issuance, amendment or
renewal of CTO
function & contact information of the review panels
right of the person subject to the CTO to apply for a
review panel hearing to cancel a CTO
only for person subject to CTO or their SDM
F. Amendment Considerations
(MHA s. 9.4)
•
A CTO can be amended by a QHP.
•
An amendment must be on Form 21 with copy of most
recent CTO (Form 19 or 20) attached.
•
If medication is stated by class (e.g.,
“antidepressant
”
in Part III of a Form 19 or 20), adjustments within that
class of medication do not require an amendment.
G. Cancellation/Expiry
(MHA s.9.2, s.9.5; CTO Reg. 8(2))
•
A CTO can only be cancelled by a psychiatrist, revi ew
panel decision, or Court of King
’s Bench.
•
If the supervising QHP is not a psychiatrist,
consultation with a psychiatrist when CTO criteria no
longer met is required to complete Form 22.
•
Supervising QHP to issue notice of the expiry of a
CTO on Form 22
.
•
All individuals notified of the issuance, amendment or
renewal of a CTO (see E), as well as the physician or
nurse practitioner who treats the person in their
ordinary day-to-day health care needs (if known)
requires notification of expiry or cancellation, along
with any recommendations for treatment.
H. Review Panel
(MHA s.34-43; CTO Reg. 9(1))
•
The person subject to a CTO or anyone on their
behalf, may apply for a review panel hearing via Form
12 to cancel a CTO
.
•
Review panel is composed of a chair or vice-chair
(must be lawyers), a psychiatrist & a member of the
public.
•
Review panel to be held within 21 days of the chair
receiving the application, and their decision to be
issued within 48 hours of the hearing.
•
The person subject to a CTO has the right to legal
representation at all review panel hearings.
•
Issuing QHP to send copy of renewal forms to review
panel for deemed applications.
•
Any decision or order of the review panel may be
appealed to the Court of
King’s Bench.
I. Non CTO Clinical Considerations
•
When a person does not meet the criteria for a CTO,
the CTO has expired or has been cancelled, care
providers should consider:
need for hospital admission either as a formal
patient (see MHA s.2 for admission criteria) or as
a voluntary patient.
any
treatment recommendations the person may
be willing to accept voluntarily
.
Additional Information
•
Informed consent to treatment is a separate process
from consent to CTO.
•
Treatment providers are responsible to obtain and
appropriately document informed consent for the
treatment they provide.
•
In addition to the prescribed MHA forms referenced, all
providers are expected to follow professional standards
and organizational guidelines for documentation.

Classification: Protected A 107
CHAPTER 8: Confidentiality and Access to
Information
This chapter will cover
• what is the purpose of the Health Information Act,
• what is common terminology,
• who can access health information,
• when access to health information may be denied,
• when health information can be used and disclosed without patient consent,
• what considerations are given to minors’ requests to access health information, and
• questions about access, use and disclosure of health information in practice.
8.1 Introduction to the Health Information Act (the “HIA”)
Given the personal and sensitive nature of psychiatric and mental health related
information, the Mental Health Act provides numerous safeguards, largely noted in
section 17. The HIA provisions also apply.
Section 17(1)(b) defines “diagnostic and treatment centre” or “centre” as “a place
established by the Minister pursuant to section 49(1)(a) or (b) and includes a facility that
is not an approved hospital under the Hospitals Act and a hospital under the jurisdiction
of a provincial health board under the Regional Health Authorities Act”.
Purpose
The Health Information Act (HIA) establishes rules to protect the privacy of an
individual's health information. It also regulates how health information can be collected,
used, and disclosed.
The HIA contains rules about the collection, use and disclosure of health information by
“custodians.” The legislation’s purpose is to
• protect the privacy of individuals and confidentiality of their health information,
• ensure that health information is appropriately shared and accessed,
• prescribe rules for the collection, use and disclosure of health information,
• make certain that health records are protected, and
• provide individuals with the right to access and make corrections to their own health
information (with certain exceptions).
Terminology

Classification: Protected A 108
Familiarity with the following terms in the HIA helps those working in healthcare
understand the parameters for using and disclosing health information in practice.
The term “custodian” in the HIA, includes, among others, regional health authorities
and designated facilities (see Appendix III).
For example, currently there is only one regional health authority - Alberta
Health Services (AHS). AHS is a custodian under the HIA. Covenant
Health has been designated as a custodian under the HIA (section 2(1)(c)
of the Health Information Regulation).
The Mental Health Patient Advocate and review panels appointed under the Mental
Health Act are also designated as custodians (section 2(1) of the Health Information
Regulation).
The term “affiliate” of a custodian is defined in the HIA and includes
• employees of the custodian,
• any person that performs services for the custodian (e.g., contractor, volunteer, or
student), and
• health services providers who can admit and treat patients at hospitals (e.g.,
physicians with hospital privileges).
The term “disclosure” refers to giving health information by any means to any person
or organization external to the custodian and
• includes sending health information from one custodian to another custodian or non-
custodian, but
• does not include the sharing of information between a custodian and their
affiliate(s).
Principles
Relevant principles underlying the legislation are referred to in the Health Information
Act Guidelines and Practices Manual can be located at
https://open.alberta.ca/publications/9780778582922. The principles include:
• custodians are the trusted “gatekeepers” of an individual’s health information. They
must determine whether the amount and type of information to be collected, used,
and disclosed is necessary,
• custodians must have the necessary authority to collect, use or disclose the
information, and
• individuals (e.g., patients, minor patients in some cases, former patients,
representatives of patients) have the right (subject to some exceptions) to access
Classification: Protected A 109
their own health information, to ask that it be corrected if there are errors in it, and to
know why it is being collected.
There are numerous rules for use and disclosure of electronic health information.
Custodians must have technical and physical safeguards to protect all records and
information. The Office of the Information and Privacy Commissioner (Alberta) is
responsible for overseeing compliance with the HIA.
8.2 The Right to Access Health Information
Section 104 of the HIA identifies who has a right of access to health information, e.g.,
the health record. For instance, access to health information may be exercised by the
following individuals or authorized representative(s)
• the individual who is 18 years or older,
• an individual under 18 years of age who understands the nature of the right or
power and the consequences of exercising the right or power (note: mature minors
likely fit these criteria as may others who may not meet the full “mature minor”
criteria but meet the criteria in this clause),
• the guardian of a minor when the minor does not understand the nature of the right
or power and consequences of exercising the right or power,
• the adult patient’s guardian or trustee (if it relates to their powers under the AGTA
and proof of their right to act is provided),
• the agent of an individual under the Personal Directives Act (if the personal directive
so authorizes),
• the attorney named in an individual’s power of attorney if the exercise of the right or
power relates to the powers and duties conferred by the power of attorney. Note: it is
important to ensure that accessing the health record relates to the attorney’s
exercise of a function in the power of attorney,
• the nearest relative of a formal patient under the Mental Health Act to carry out
obligations or exercise rights under the Act, or
• by any person with the individual’s written authorization to act on their behalf, e.g.,
legal counsel.
8.3 The Right to Refuse Access to Health Information
The relationship between the Mental Health Act and the HIA is complex. For assistance
with interpretation of this legislation, ideally, legal advice should be sought.
Section 11(1)(a) of the HIA provides that a custodian may refuse to disclose health
information to an applicant if disclosure could reasonably be expected to
• result in immediate and grave harm to the applicant’s mental or physical health or
safety,
Classification: Protected A 110
• threaten the mental or physical health or safety of another individual, or
• pose a threat to public safety.
A custodian may also refuse to disclose health information to an applicant:
• if the disclosure could reasonably lead to identifying the person who provided health
information to the custodian in confidence, and
• where it is appropriate that the name of the person who provided the information be
kept confidential.
A custodian must refuse disclosure in certain circumstances. As an example, disclosure
must be refused if the health information is about an individual other than the applicant,
unless the health information was originally provided by the applicant in the context of a
health service being provided to the applicant (section 11(2) of the HIA).
8.4 Using and Disclosing Health Information in a Limited Manner
Custodians have a duty to use health information in a limited manner.
That means they are required to use and disclose the least amount of information
required for the custodian or recipient to carry out their intended purpose. Health
information is to be shared internally on a ‘need-to-know’ basis (section 58 of the HIA).
With respect to disclosure, a custodian must consider the individual’s expressed
wishes as a factor when deciding how much health information to disclose (section
58(2) of the HIA).
As an example, a formal patient in her seventh month of pregnancy is
scheduled to attend an appointment with an obstetrician. The obstetrician
has been following her throughout her pregnancy (prior to her hospital
admission) and is well aware of her psychiatric history. The patient
expresses concern about the confidential psychiatric information on her
health record and whether it is necessary for the obstetrician’s team to
have access to it. Taking into consideration the patient’s wishes and after
discussion about ‘need-to-know’ information, it is agreed within the
psychiatric team to share with the obstetrical team information relevant to
the pregnancy and her current state of physical and mental health. Such
information includes the patient’s medications, laboratory results, blood
pressure readings, her response to current treatment and any concerns or
risks. The amount of ‘need to know’ information changes with each
patient. Depending on the patient’s mental illness, relevant mental
health information may be disclosed if it affects her pregnancy.
Classification: Protected A 111
8.5 Using and Disclosing Health Information without the
Patient’s Consent
Though the following are not the only instances of use and disclosure of health
information under the HIA, they are examples commonly encountered in practice.
Healthcare providers are encouraged to refer to their facility’s or organization’s policies
prior to the disclosure of patients’ health information.
Health services under same custodian
Subject to any rules set by the custodian, the custodian’s employees who are
healthcare providers and the physicians on staff at the custodian’s facilities may share a
patient’s health information among themselves, without the patient’s consent, if it is for
the purpose of providing health services to that patient (section 27(1)(a) of the HIA).
Continuing care and treatment
It is permissible to disclose diagnostic, treatment and care information without the
individual’s consent to a person providing continuing care and treatment. This provision
is not limited to healthcare providers (section 35(1)(b) of the HIA).
Permissible disclosure would include, for instance, a parent, relative,
caregiver or friend involved in the ongoing care of a patient. It would also
include a care provider from a sector outside of health who is providing
continuing care and treatment.
There are mandatory provisions for disclosure upon discharge in the Mental Health Act
discussed below (Notification of Discharge). The discretionary provisions in section
35(1)(b) of the HIA allow for information to be sent to those persons who are
responsible for providing continuing care and treatment.
Risk of Harm
A provision in the HIA permits a custodian to disclose health information without
consent to any person if the custodian believes on reasonable grounds that the
disclosure will avert or minimize:
(i) a risk of harm to the health or safety of a minor, or
(ii) a significant risk of harm to the health or safety of any person (section 35(1)(m)
of the HIA).
To protect public health and safety
A custodian has discretionary authority to disclose limited identifying health information
without the individual’s consent to the police or the Minister of Justice and the Attorney
General where the custodian reasonably believes:
Classification: Protected A 112
• the information relates to a possible commission of an offence under a statute of
Alberta or Canada, and
• the disclosure will protect the health and safety of Albertans (section 37.3 of the
HIA).
In this instance, if a healthcare provider employed by or contracted with
AHS does not want to disclose to the police and wants to disclose to the
Minister, the healthcare provider can contact AHS Legal for information
about who in the Ministry to contact. Otherwise, the healthcare provider
can contact the Minister’s office to be directed to the appropriate person.
The limited amount of information that can be disclosed is as follows:
(a) name of an individual,
(b) date of birth of an individual,
(c) nature of any injury or illness of an individual,
(d) date on which a health service was sought or received by an individual,
(e) location where an individual sought or received a health service,
(f) whether any samples of bodily substances were taken from an individual.
Disclosure to the medical examiner’s office
When a formal patient dies the medical examiner must be notified (sections 11(b) and
12(b) of the Fatality Inquiries Act).
In practice, if a formal patient dies in a facility, the medical examiner (ME)
comes to the unit where the death occurred. As part of the ME’s
investigation, the ME asks to view the current health record. If the death of
the formal patient occurs outside the facility (e.g., while the patient is on a
pass/leave from hospital), the ME is notified as soon as the patient’s death
is reported to the facility. In this case, the ME also requests access to the
health record. Furthermore, the ME can ask to review the health record of
any mental health patient who died unexpectedly post discharge.
Health records can be disclosed to the MEs office pursuant to section 35(1)(p) of the
HIA (authorizing disclosure without consent if the disclosure is authorized or required by
an Act of Alberta or Canada) together with section 21(3) of the Fatality Inquiries Act
which provides
21(3) Notwithstanding any other Act, regulation or other law, a medical examiner is
entitled to inspect and make copies of any diagnosis, record or information relating
to
(a) a person receiving diagnostic and treatment services in a diagnostic and
treatment centre under the Mental Health Act, or
Classification: Protected A 113
(b) a patient under the Hospitals Act.
Special rules for disclosure to police by emergency medical services
The Emergency Health Services Act provides for the disclosure of certain information by
ambulance attendants to peace officers without the consent of the patient. Such
information includes but is not limited to the nature of a patient’s illness, which includes
mental illness.
Special rules for disclosure of gunshot and stab wounds
The Gunshot and Stab Wound Mandatory Disclosure Act mandates that staff working in
healthcare facilities and emergency medical technicians report certain information to the
local police service when a gunshot or stab wound is treated (or treatment is offered).
Reporting is not required if staff or EMTs reasonably believe that the stab wound is self-
inflicted or unintentionally inflicted. Reporting will include only limited patient information,
e.g., patient’s name, the healthcare facility and type of wound but no treatment or
diagnostic information. For more information on this legislation and the specified
information that must be disclosed, healthcare providers are encouraged to contact their
internal legal counsel.
Disclosure of information provisions in the Mental Health Act
Readers are encouraged to view section 17 of the Mental Health Act in its entirety for
other situations where health information can be disclosed without patient consent (e.g.,
to the Public Guardian, Public Trustee, review panel, Director of Medical Services under
the Occupational Health and Safety Act, the Workers’ Compensation Board, the
Department of Health (Canada), Review Board appointed pursuant to the Criminal Code
(Canada), Council of College of Physicians and Surgeons of Alberta, a hearings director
of a college under the Health Professions Act, etc.).
Notification of Discharge
Provisions for notifying individuals of a patient’s discharge without patient consent are
covered both in the Mental Health Act and the HIA.
Mental Health Act
The notification provisions in section 17(9) and section 32 of the Act apply to all
patients, including voluntary and formal patients.
a) Section 17(9)
• When a patient is discharged from a diagnostic and treatment centre for the
purposes of transferring them to another treatment centre, hospital or nursing
Classification: Protected A 114
home, copies of the appropriate records of diagnostic and treatment services
provided to that patient are forwarded for use at the receiving facility.
b) Section 32
• Notification of discharge is covered in Section 32 of the Act which states that,
when reasonably possible, a patient’s nearest relative must be notified of the
patient’s discharge if the patient does not object on reasonable grounds.
- As an example, this could apply when a voluntary patient discharges
themself against medical advice if the patient had not previously voiced an
objection.
• Similarly, when reasonably possible, the patient’s guardian is to be given notice
of discharge. This would apply in all guardianship circumstances (e.g., the AGTA,
guardians of minors under the Child, Youth and Family Enhancement Act, or
parent guardians of minors).
• Section 32 of the Act requires notification of the family physician or nurse
practitioner who treats the patient in their ordinary day-to-day health care needs,
if known, on a patient’s discharge. As well, a discharge summary and any
recommendations for treatment are to be sent.
• With all notifications under section 32 of the Act, when applicable a statement
shall be included regarding whether a certificate of incapacity issued under the
Public Trustee Act exists with respect to the patient.
Health Information Act
• Discharge notification may be disclosed to a caregiver who is involved in the
continuing care of the patient (section 35(1)(b) of the HIA).
- For instance, an aunt who drives her nephew to a clinic for bi-weekly
mental health follow-up may be advised of the patient’s discharge. A
worker in a Group Home could be notified of a patient’s date of discharge
and return to that facility.
8.6 Disclosure of Health Information with Consent
A person’s health information can also be disclosed with their consent. Their consent
must meet the requirements set out in section 34 of the HIA. Healthcare providers are
encouraged to refer to their applicable policies and use their organization’s standard
consent form.
Classification: Protected A 115
8.7 Questions about Access, Use and Disclosure of Health
Information in Practice
1. What information is disclosed to the physician or nurse practitioner who treats
the patient in their ordinary day-to-day health care needs on a patient’s
discharge?
Section 32 of the Act directs that, when reasonably possible, notice of the patient’s
discharge must be provided to the physician or nurse practitioner who treats the patient
in their ordinary day-to-day health care needs, including a discharge summary and any
recommendations for treatment. Additionally, when applicable, the discharge
information is to identify whether a Certificate of Incapacity (issued under the Public
Trustee Act) exists with respect to the patient.
(Note: all the existing Certificates of Incapacity formerly issued under the Dependent
Adults Act were transferred to the Public Trustee Act in October of 2009 when the
Dependent Adults Act was repealed.)
The Act does not require the patient’s consent in this instance. Some clinicians advise
the patient that a discharge summary is being sent to their physician or nurse
practitioner who treats the patient in their ordinary day-to-day health care needs though
notifying the patient is not a requirement under the Act.
Health information may also be provided to a person who is responsible for providing
continuing treatment and care to the individual (section 35(1)(b) of the HIA), such as a
mental health clinic where the person received services prior to admission.
2. What if a patient specifically instructs their qualified health practitioner not to
send discharge notice and follow-up information to the family physician or
nurse practitioner who treats the patient in their ordinary day-to-day health
care needs?
It is a requirement under the law for the discharge notice, discharge summary, and
recommendations for treatment (and when applicable the identification of whether a
Certificate of Incapacity is in effect under the Public Trustee Act) to be sent to the family
physician or nurse practitioner who treats the patient in their ordinary day-to-day health
care needs, where reasonably possible. Therefore, this information must be sent even if
it is against a patient’s wishes. The healthcare team would be encouraged to speak with
the patient to explore the reasoning behind their request.
3. Can formal patients view their current health record?
Yes, patients have right of access by completing a written request unless the exceptions
set out in section 11 of the HIA apply. For instance, under section 11(1)(a), access to
the record would be denied if it would result in immediate and grave harm to the
Classification: Protected A 116
applicant’s mental or physical health or safety, threaten the mental or physical health or
safety of another individual, or pose a threat to public safety.
Note: A formal patient does not need to make a request for their medical records if they
have made an application to the review panel (per section 14(6) of the MHA.
Readers with questions are encouraged to contact their organization’s Information
and Privacy department and reference their organization’s policies.
4. How should healthcare providers respond when a formal patient asks to read
their current health record?
In practice, if the patient asks staff about reading their chart, it is helpful if staff inform
the attending physician of the patient’s request so the physician and patient can discuss
it.
Affiliates (e.g., employees) should contact the Information and Privacy department at
their facility for clarification of the patient’s rights in these situations or indeed, when any
concerns or uncertainty exist (e.g., about information on the health record that may be
detrimental to the patient or another person).
Many physicians prefer to be with the patient at the time of reading health information to
explain any entries or language that is not understood and to answer any questions that
arise.
5. Can patients under the age of 18 (including formal patients who are minors,
minors who are subject to CTOs, voluntary patients who are minors and
mature minors) request access to their health record?
It depends. Minors (whether formal patients or not) can exercise their own rights under
HIA if they understand the nature of the right and the consequences of exercising that
right.
To determine whether a person under the age of 18 is a mature minor capable of
understanding the nature and consequences of exercising their rights or powers under
the HIA, the following factors are considered
• the individual’s age,
• maturity,
• independence,
• level of understanding, and
• the nature and complexity of the HIA rights or powers.
The Privacy Commissioner ruled that the level of understanding that is required for an
individual to understand the nature and consequences of exercising rights or powers
Classification: Protected A 117
under the HIA is not a particularly onerous standard (OIPC Order F2005-017 and
H2005-001).
If the minor does not understand the nature of their rights and consequences under the
HIA, then their guardian can exercise those rights (section 104(1)(c) of the HIA).
If healthcare providers need guidance whether a mature minor under the Act can
expressly preclude their guardian from obtaining the mature minor’s health information,
they should seek guidance from their organization’s internal legal counsel.
6. Can staff and physicians answer questions from family or friends about the
diagnosis and treatment of formal patients?
• The HIA provides that so long as disclosure is not contrary to the patient’s
expressed wishes, the custodian may provide limited information to persons in a
close personal relationship with the patient without the patient’s consent.
Information such as the patient’s location, diagnosis, progress, prognosis, and
condition on that day may be disclosed to persons in a close personal
relationship with the patient. “Close personal relationship” could include common-
law spouse, friend or person who can demonstrate they have such a relationship
with the patient (section 35(1)(c) of the HIA).
• Section 14(1) of the Mental Health Act addresses disclosing information as well.
For instance, notifications of a formal patient’s certification and of the formal
patient’s rights are provided to the patient’s nearest relative, unless the patient
objects on reasonable grounds. Formal patients are also asked to designate a
person they wish to receive the written statement and copies of the information
required in sections 14(1)(b) and 14(1)(c) of the Act. There are also
circumstances in which regular communication is expected of the team and is
allowed. This is the case in disclosure of information to guardians of formal and
voluntary patients - whether they are guardians under the AGTA or guardians of
patients who are minors.
• Note: similar provisions for disclosing information exist beyond section 14(1) across the Act (e.g.,
18(1), 32(1)(b) and CTO Regulation section 7(3).
• Similarly, the team can engage in treatment-related communication with agents
and SDMs under section 28 of the Mental Health Act.
- In general, if a healthcare provider is uncertain about the patient’s wishes,
it is good practice to inform the competent patient about the information
request and ask the patient for their consent. Some patients may stipulate
conditions. They may ask, as is their right, that specific information not be
discussed with an identified person. (This expressed wish would be

Classification: Protected A 118
granted provided the identified person is not the patient’s SDM under
section 28 of the Act.)
If a healthcare provider is concerned about conflict, or unsure about disclosure or
refraining from disclosing health information, they are encouraged to seek legal advice
from their organization’s internal legal counsel or Canadian Medical Protective
Association as appropriate.
7. What should healthcare providers do when they are uncertain whether or not
they can call the police, how much information they can tell the police, and
whether they have a duty to call the police.
Healthcare providers are encouraged to consult their organization’s legal counsel (e.g.,
AHS Legal Services) or Information and Privacy department if they need guidance
regarding 1) whether they have an obligation to disclose given the particular
circumstances and 2) how much information to disclose.
Readers can review the comprehensive Alberta Health publication (2018), Health
Information Act - Guidelines and Practices Manual (“HIA Guidelines and Practices
Manual”), available at: https://open.alberta.ca/publications/9780778582922
Classification: Protected A 119
CHAPTER 9: Mental Health Patient Advocate
This chapter will cover
• what is the jurisdiction of the Patient Advocate,
• which complaints the Patient Advocate can investigate,
• what the Patient Advocate can investigate without a complaint,
• what rights advice is given,
• who investigates complaints,
• what are the notification requirements,
• when the Patient Advocate may refuse to investigate,
• how an investigation is conducted,
• what information does the designated facility provide the Patient Advocate,
• how confidentiality is maintained during the investigation,
• who receives the report at the end of an investigation,
• how to contact the Patient Advocate, and
• questions about the Patient Advocate in practice.
Introduction
Sections 44 through 47 of the Act together with the Mental Health Patient Advocate
Regulation under the Act provide for the Lieutenant Governor in Council to appoint a
Mental Health Patient Advocate (the Patient Advocate) to provide rights advice and act
as an investigative body.
The Mental Health Patient Advocate is appointed by the Lieutenant Governor in Council
(Mental Health Act RSA 2000, c M13 (“MHA”), s 45(1) and operates independently of
the government. The Mental Health Patient Advocate Regulation defines a “patient” as
a person who
a) is or has been a formal patient,
b) is or has been subject to one admission certificate, or
c) is or has been subject to a community treatment order.
A complaint may be investigated by the Patient Advocate or an employee of the Patient
Advocate. Employees may be appointed to assist the Advocate (section 46(1) of the
Act). The Patient Advocate may in writing delegate to any person any power or duty
under the Act or the Mental Health Patient Advocate Regulation, except for the power or
duty to make a report (section 2 of the Mental Health Patient Advocate Regulation).
In this chapter, the term “patient” will have the same meaning as in the
regulation.
Classification: Protected A 120
9.1 Jurisdiction
The Patient Advocate is the only provincial investigative body created specifically to
deal with complaints from or relating to persons detained in designated facilities under
one or two admission or renewal certificates, and persons subject to a community
treatment order (CTO).
The Patient Advocate’s roles and responsibilities are found in section 45 of the Act
together with the Mental Health Patient Advocate Regulation. The Patient Advocate is
specifically authorized to conduct an investigation with or without a complaint and
provide rights advice.
9.2 Investigations Based on Complaints
The Patient Advocate has jurisdiction to investigate complaints from or relating to
• patients under one admission certificate,
• formal patients (patients under two admission certificates, or two renewal
certificates), and
• persons who are subject to a CTO.
The Patient Advocate does not have the jurisdiction to investigate complaints regarding
voluntary patients. Section 6(5) of the Mental Health Patient Advocate Regulation limits
the Patient Advocate’s investigation to the period during which the person was subject
to one or two admission certificates, one or two renewal certificates, or a CTO.
If, for example, the Patient Advocate received a complaint following the
discharge of a previously formal patient, the investigation could
encompass the time from the issuance of the first admission certificate
through to the cancellation or expiration of the last two admission or
renewal certificates issued for the patient during that hospitalization.
9.3 Investigations without a Complaint
Without receiving a complaint, section 4(1) of the Mental Health Patient Advocate
Regulation enables the Patient Advocate to initiate and conduct an investigation into
any matter under the Act relating to a patient with or without the patient’s consent.
Further, without receiving a complaint the Patient Advocate may initiate and conduct an
investigation into
• any procedure relating to the admission of a person detained in a facility
pursuant to the Act,
• any procedure for 1) informing a patient of their rights, or 2) providing information
as required by the Act to a patient and to guardians, nearest relative or
designates of a patient, and
Classification: Protected A 121
• any procedure of a regional health authority or issuing qualified health
professional relating to the issuance, amendment, or renewal of a CTO.
9.4 Rights Advice
Section 45(1.1) of the Act requires the Patient Advocate to contact each formal patient
who has requested contact as soon as practicable after receipt of the patient’s
admission certificates or renewal certificates. The Patient Advocate may provide to each
formal patient, the patient’s guardian, if any, one person designated by the patient and,
unless the patient objects, the patient’s nearest relative, information respecting:
• the authority for the patient’s detention and the period of it,
• the function of review panels,
• the name and address of the chair of the review panel for the facility,
• the right to apply to a review panel for cancellation of the admission certificates
or renewal certificates or for an order for the board to issue a community
treatment order, and
• the right of a patient to free and timely access to their medical records relevant to
a hearing before a review panel or the Court of King’s Bench.
The Patient Advocate must ensure that all formal patients have been provided complete
information by the board under section 14 of the Act.
As well, the Patient Advocate must review the summary of information provided by the
board under section 14 of the Act with the formal patient.
The Patient Advocate may contact and advise a formal patient or a person who is
subject to a CTO at any time, regardless of whether a complaint has been received from
or relating to the formal patient or person who is subject to a CTO (section 45(1.2) of the
Act).
After receiving a complaint or initiating an investigation without a complaint into any
matter under the Act relating to a patient, section 6(2) of the Mental Health Patient
Advocate Regulation requires that the Patient Advocate provide to the complainant or
the patient to whom a matter under investigation relates, as far as is reasonable,
information about:
• the patient's rights under the Act,
• how the patient may obtain free legal services,
• how the patient may apply to the review panel,
• how the patient can commence an appeal to the Court of King's Bench.
Classification: Protected A 122
9.5 Notification Requirements
Section 5(1) and section 5(5) of the Mental Health Patient Advocate Regulation provide
that the Patient Advocate must issue a notice of investigation as follows:
• notify the board of the facility where the patient is or was detained that an
investigation has been initiated and the nature of the matter or complaint under
investigation,
• if a patient has been transferred, notify the board of both facilities,
• notify the patient in writing if the Patient Advocate is conducting an investigation
without complaint under section 4(1) of the Mental Health Patient Advocate
Regulation that an investigation has been initiated and the nature of the matter
under investigation,
• notify the patient in writing that a complaint has been received, the nature of the
complaint, and any investigation arising from the complaint, and
• if an individual other than the patient is named in a complaint, notify the individual
of any investigation arising.
In addition, section 5(2) of the Mental Health Patient Advocate Regulation requires that
the Patient Advocate notify the board of the facility of the Patient Advocate’s intention to
contact a patient of the facility.
Where the Patient Advocate investigates without complaint a procedure that relates to a
facility, the Patient Advocate must notify the board of the facility (section 5(3) of the
Mental Health Patient Advocate Regulation).
The Patient Advocate must notify the regional health authority or issuing qualified health
professional of the Patient Advocate’s investigation relating to that regional health
authority or qualified health professional (section 5(4) of the Mental Health Patient
Advocate Regulation).
9.6 Refusal to Investigate
The Patient Advocate may refuse to investigate or cease to investigate a matter if the
Patient Advocate believes that the subject matter of the complaint is trivial, the
complaint is frivolous or vexatious, no investigation is necessary having regard to all of
the circumstances, or the subject-matter is more appropriately addressed by a different
committee, body, person or other entity (section 9(1) of the Mental Health Patient
Advocate Regulation).
The Patient Advocate may, with the consent of the complainant, attempt to resolve the
complaint without an investigation (section 9(2)(a) of the Mental Health Patient
Advocate Regulation). Referrals to a committee, body, person, or other entity with
authority to investigate may be made with the consent of the complainant or the patient
Classification: Protected A 123
to whom a matter or patient complaint relates (section 9(2)(b) of the Mental Health
Patient Advocate Regulation).
9.7 Conduct of Investigation
The Patient Advocate has discretion about how to conduct the investigation.
• The Patient Advocate may make any inquiries that the Patient Advocate
considers necessary (section 6(1)(b) of the Mental Health Patient Advocate
Regulation).
• The Patient Advocate is authorized to make any contact with the patient and
conduct any investigation the Patient Advocate considers necessary (section
6(1)(c) of the Mental Health Patient Advocate Regulation).
• The Patient Advocate is not required to hold a hearing (section 6(4) of the Mental
Health Patient Advocate Regulation).
9.8 Conduct of Investigation; Right to Make Representations
The patient and the person who have been named in a complaint and have received
notification of an investigation have the right to make representations to the Patient
Advocate (section 6(3) of the Mental Health Patient Advocate Regulation).
9.9 Conduct of Investigation; Cooperation by the Facility
Upon request, a facility, board, regional health authority or issuing qualified health
professional must provide to the Patient Advocate within a reasonable time (section
11(1) of the Mental Health Patient Advocate Regulation):
• any of their policies or directives or other documents relating to an investigation,
and
• any medical or other record or any information, file or other document relating to
a patient who is the subject of an investigation or to whom an investigation
relates.
If the board is notified of the Patient Advocate’s intention to contact a patient, the board
must grant the Patient Advocate access to the patient at all reasonable times (section
12(a) of the Mental Health Patient Advocate Regulation). The board must grant the
Patient Advocate access to a formal patient at all reasonable times for all the purposes
set out in section 45 of the Act (section 12(b) of the Mental Health Patient Advocate
Regulation).
Classification: Protected A 124
9.10 Confidentiality of Information Obtained During the
Investigation
The Patient Advocate must not disclose information obtained during an investigation
except as required by law or in the performance of the Patient Advocate’s duties under
the Act or Regulation (section 7 of the Mental Health Patient Advocate Regulation).
9.11 Record of Investigation
The Patient Advocate must maintain a record of every complaint and investigation
(section 6(1)(a) of the Mental Health Patient Advocate Regulation).
9.12 Reporting at the End of an Investigation
The Patient Advocate must provide the board, regional health authority, or issuing
qualified health professional with a copy of the Patient Advocate’s investigation report
(section 8(1) of the Mental Health Patient Advocate Regulation).
If the report contains recommendations, it must state the reasons for the
recommendations (section 8(2) of the Mental Health Patient Advocate Regulation).
Should the Patient Advocate believe that the board, regional health authority, or issuing
qualified health professional has not taken appropriate action within a reasonable time
on any recommendation, the Patient Advocate must send a copy of the report and any
response to the Minister (section 8(3) of the Mental Health Patient Advocate
Regulation).
The Patient Advocate must inform a patient of the disposition of any patient complaint
(section 10(a) of the Mental Health Patient Advocate Regulation).
The Patient Advocate may inform a complainant of the disposition of any complaint they
initiate (section 10(b) of the Mental Health Patient Advocate Regulation).
The Patient Advocate may inform a patient of the disposition of any matter initiated
without a complaint under section 4(1) of the Mental Health Patient Advocate
Regulation that relates to the patient (section 10(c) of the Mental Health Patient
Advocate Regulation).
9.13 Contact Information
The Patient Advocate can be contacted through the Office of the Alberta Health
Advocates as follows:
The telephone number in Edmonton is 780-422-1812. This number can be accessed
outside Edmonton toll-free at 310-0000 then dial 780-422-1812. A confidential
answering machine is available to those who call outside of the office hours.
Classification: Protected A 125
The office is open from 8:15 a.m. to 4:30 p.m. from Monday through Friday, except
statutory holidays.
The address is 9th Floor, 10055 – 106 Street, Edmonton, Alberta T5J 2Y2.
9.14 Questions about the Mental Health Patient Advocate in
Practice
1. Do complaints to the Patient Advocate have to be written or be in any
particular form?
Complaints and concerns may be communicated by phone, email, online inquiry form,
in writing by mail, or in person by visiting the Patient Advocate’s office in Edmonton.
2. Within what time frame must the facility provide information to the Patient
Advocate?
Under section 14(1)(d) of the Act, if a formal patient requests to be contacted by the
Patient Advocate, the board shall notify the Patient Advocate and provide the Patient
Advocate with copies of the certificates and information. There is no specific timeline for
this information to be communicated by the board to the Patient Advocate. Section
45(1.1)(a) provides the Patient Advocate shall contact the formal patient as soon as
practicable after receipt of the certificates. Copies of materials requested by the Patient
Advocate must be provided to the Patient Advocate within a ‘reasonable time’ (section
11 of the Mental Health Patient Advocate Regulation). The Patient Advocate provides
timelines in the written notification letter advising the facility to supply the Patient
Advocate with the required information.
In addition, timelines for response to any recommendations are outlined in the Patient
Advocate’s report of the investigation sent to the board of the facility. The written
response to the Patient Advocate’s recommendations by the board of the facility must
meet the timelines. Should a recommendation require more time to implement than that
given, the Patient Advocate should be advised of progress made at the time of the
written response.
3. Can the Patient Advocate, when investigating designated facility procedures,
access health records and interview formal patients if no complaint has been
received?
Yes, if accessing the health records and/or interviewing the formal patient relates to the
Patient Advocate’s investigation. The Patient Advocate has broad discretion and can
make inquiries that the Patient Advocate considers necessary to conduct an
investigation (section 6(1)(b) of the Mental Health Patient Advocate Regulation and
section 45(3) of the Act.)
Classification: Protected A 126
4(a). A qualified health professional issues a Form 1 - Admission Certificate on a
patient who is taken to a designated facility for examination. The patient
subsequently lodges a complaint with the Patient Advocate. Can the
Patient Advocate, in the course of an investigation, ask for information
from the issuing qualified health professional?
Yes.
What information can be accessed?
The Patient Advocate is designated as a “custodian” under the HIA (section 2(1) of the
Health Information Regulation). Health information may be disclosed by the qualified
health professional that issued the Form 1 to the Patient Advocate pursuant to sections
35(1)(a) and 27(1)(f) of the HIA.
4(b). What if the patient’s family, rather than the patient, asked the Patient
Advocate to look into the admission of the patient as a formal patient?
Yes, section 45(1.1)(e) of the Act and section 1(b) and 3 of the Regulation do not
specify that a complaint needs to be made by a patient, only that a complaint must be
made relating to a patient.

Classification: Protected A 127
APPENDIX I: Glossary
Glossary
Glossary contains only key terms found in this guide.
ACT
In this guide the “Act” means the Mental Health Act (Alberta).
ADMISSION CERTIFICATE
A certificate issued under section 2 or 3 of the Act by a qualified health professional who
believes a person (section 1(1)(a) of the Act):
• is suffering from mental disorder,
• has the potential to benefit from treatment for the mental disorder,
• is, within a reasonable time, likely to cause harm to others or to suffer negative
effects, including substantial mental or physical deterioration or serious physical
impairment, as a result of or related to the mental disorder, and
• is unsuitable for admission to a facility other than as a formal patient.
An admission certificate may also be issued under section 3 of the Act for a person
detained under the Criminal Code of Canada or Youth Criminal Justice Act (of Canada).
AGENT
This term is defined under section 1(1)(a) of the Personal Directives Act (Alberta) as a
person designated in a personal directive to make decisions on behalf of a person who
completes a personal directive.
These decisions may involve healthcare matters, including examinations, procedures,
services, or treatments completed for therapeutic, preventive, palliative, diagnostic or
other purposes.
The Personal Directives Act is available at the Government of Alberta, King’s Printer,
Laws Online Results website: https://kings-printer.alberta.ca/Laws_online.cfm. Once on
the website, search by title for the Personal Directives Act or
https://open.alberta.ca/publications/p06.
COMMUNITY TREATMENT ORDER (CTO)
An order issued by two qualified health professionals (one of whom must be a
psychiatrist) if a person meets certain criteria and they believe the person will
experience recurring relapses and hospitalizations (frequently as formal patients under
the Act) if the person does not receive the required community treatment or care.

Classification: Protected A 128
CORRECTIONAL FACILITY
Correctional Facility is not defined in the Act.
In the Corrections Act, correctional institution is defined as:
(i) a holding or lock-up facility operated by the police on a daily fee or a fee for service
basis for the purpose of confining persons being held in custody prior to court
appearances, on remand or undergoing a sentence or sentences of imprisonment
either imposed by a court in Alberta, or imposed elsewhere than in Alberta when
those persons are transferred to Alberta pursuant to an Act of Canada or an Act of
another province or territory,
(ii) a detention or remand facility operated by or for the Government of Alberta to detain
arrested, charged or convicted persons pursuant to a law in force in Alberta,
(iii) a forestry or similar facility operated by the Government of Alberta,
(iv) a jail or institution referred to in section 6(1), or
(v) any other facility designated as a correctional institution by the Minister
but does not include a secure services facility within the meaning of the Child, Youth
and Family Enhancement Act.
The Mental Health Act refers to a Correctional Facility (section 33 of the Act) and a
Custodial Institution (section 9.1 of the Act, dealing with CTOs), rather than a
Correctional Facility. A Custodial Institution likely has a broader meaning than a
Correctional Facility. For example, an open custody group home for youth may be a
‘custodial institution’ but not a correctional facility.
FACILITY
“A place or part of a place designated in the regulations as a facility” (section 1(1)(d) of
the Act). In practice the term refers to inpatient health facilities which have been
designated by the Minister pursuant to section 52(1.1) of the Act as the only places
which can admit and detain formal or involuntary patients under the Mental Health Act.
There are many hospitals in Alberta but only a limited number are designated facilities
under the Mental Health Act Forms and Designation Regulation. A list of these facilities
as of April 2021 is in Appendix II (section 15.2(1) of the Mental Health Forms and
Designation Regulation 136/2004).
FORMAL PATIENT
A patient detained in a facility pursuant to two admission certificates (section 2 and 3 of
the Act) or two renewal certificates (sections 8 and 9 of the Act).

Classification: Protected A 129
GUARDIAN
Under the Mental Health Act
• the parent or guardian of a minor,
• a director as defined in the Child, Youth and Family Enhancement Act for a child
who is subject to a temporary or permanent guardianship order, or permanent
guardianship agreement,
• a guardian appointed under the Adult Guardianship and Trusteeship Act who has
the authority to act and make decisions with respect to
- the adult’s health care
- carrying on any legal proceeding that does not relate primarily to the estate of
the adult.
Under the Adult Guardianship and Trusteeship Act
• An individual appointed by a court to make decisions for an adult, acting in their
best interests, whose interests will not conflict with the adult’s interests.
• A Guardian is appointed under the Adult Guardianship and Trusteeship Act
where the Court is satisfied that an adult does not have capacity to make
decisions about personal matters and other less intrusive measures would not
likely be or have not been effective.
• Usually among the Guardian’s powers and authorities is the power to consent to
any health care that is in the adult’s best interests.
• The Adult Guardianship and Trusteeship Act and its Regulations are located at
the Government of Alberta, King’s Printer, Laws Online Results website:
https://kings-printer.alberta.ca/Laws_online.cfm. Complete a search by title: Adult
Guardianship and Trustee Act or https://open.alberta.ca/publications/a04p2 .
MENTAL DISORDER
Mental disorder is defined as a substantial disorder of thought, mood, perception,
orientation, or memory that grossly impairs judgment, behaviour, capacity to recognize
reality, or ability to meet the ordinary demands of life, but does not include a disorder
in which the resulting impairment is persistent and is caused solely by an
acquired or congenital irreversible brain injury. The change to the definition (bolded
above) which took effect on March 31, 2021, is supported by definitions in section 2.1 of
the Mental Health Regulation as follows:
(a) “irreversible brain injury” means a permanent disruption to the
baseline function of the brain or to the structure of the brain caused
or likely caused by an identifiable or probable
Classification: Protected A 130
(i) acute external action, including trauma, or
(ii) pathophysiological event within the body, including an acute
hypoxic event, but does not include a permanent disruption
caused or likely caused by a neurodegenerative disorder;
(b) “persistent” means stable and unlikely to improve as a result of
treatment.
MINISTER
Minister means the Minister of Health, who has been designated under section 16 of the
Government Organization Act as the Minister responsible for the Mental Health Act.
NEAREST RELATIVE
For a formal patient or a person subject to a community treatment order - in descending
priority order, the person’s
• spouse or adult interdependent partner,
• son or daughter,
• father or mother,
• brother or sister,
• grandfather or grandmother,
• grandson or granddaughter,
• uncle or aunt,
• nephew or niece.
(Refer to section 1(1)(i)(ii) of the Mental Health Act for more information if there is no
person within the above description, or the person determined as above would not or is
not acting in the best interest of the formal patient or person subject to a CTO.)
PATIENT
In the Mental Health Act, “patient” means a person who is admitted to a facility as an
inpatient or as an outpatient for diagnosis or treatment services, or both.
In this guide, the term “patient” is primarily used as defined in the Act. It is, however,
also used more broadly at times e.g., to refer to persons subject to community treatment
orders. The meaning of the word “patient” will depend on the context.
PEACE OFFICER
Although the Mental Health Act does not define “peace officer”, the Police Act and
Peace Officer Act do. The Minister responsible for both statutes is the Minister of
Justice and Solicitor General.
Classification: Protected A 131
Section 7 of the Peace Officer Act provides that the Minister of Justice and Solicitor
General can appoint a person as a peace officer to hold broad or limited authorities,
dependent on job functions.
PERSONAL DIRECTIVE
A legal document that sets out advanced personal instructions for an individual, and
which may designate a person to make decisions on behalf of the individual, regarding
personal matters as defined in the Personal Directives Act (section 1(k) and Part 2).
The website reference is located at the Government of Alberta, King’s Printer, Laws
Online Results: https://kings-printer.alberta.ca/Laws_online.cfm. Complete a search by
title: Personal Directives Act or https://open.alberta.ca/publications/p06.
PUBLIC GUARDIAN
The person appointed as the Public Guardian pursuant to the Adult Guardianship and
Trusteeship Act.
Under section 107 of the Adult Guardianship and Trusteeship Act, the Public Guardian
means a Provincial Government staff member appointed to attend to the circumstances
of persons needing a guardian, where no individuals are willing, able, and suitable.
The website reference is located at the Government of Alberta, King’s Printer, Laws
Online Results: https://kings-printer.alberta.ca/Laws_online.cfm. Complete a search by
title: Adult Guardianship and Trusteeship Act
QUALIFIED HEALTH PROFESSIONAL
The Minister may designate in the future other qualified health professionals under the
regulations but at the time of publication of the guide, a qualified health professional is a
psychiatrist, physician, or nurse practitioner.
REGIONAL HEALTH AUTHORITY
An organization created pursuant to the Regional Health Authorities Act and
subsequent Ministerial Orders. Alberta Health Services derives its authority from this
legislation and is the only regional health authority.
A copy of this Act can be found on the Government of Alberta, King’s Printer, Laws
Online Results website: https://kings-printer.alberta.ca/Laws_online.cfm. Complete a
search by title: Regional Health Authorities Act or
https://open.alberta.ca/publications/r10.
Classification: Protected A 132
RENEWAL CERTIFICATE
A certificate issued pursuant to section 8 of the Act (section 1(1)(o) of the Act). This
provides a mechanism for extending a formal patient’s period of detention, after two
qualified health professionals who have separately examined a formal patient, believe
that formal patient meets the criteria and requires continuing psychiatric care. At least
one of the qualified health professionals who issue renewal certificates must be a
member of the staff of the designated facility at which the formal patient is detained and
at least one of the renewal certificates must be issued by a psychiatrist (section 8(2) of
the Act).
REVIEW PANELS
Three-member panels established pursuant to section 34 of the Act to hear the
following applications
• to review a certificate of incompetence to make treatment decisions, signed by a
physician (section 27 of the Act),
• from a physician for a treatment order (section 29 of the Act),
• to transfer a person back to a correctional facility (section 33 of the Act),
• to review/cancel admission certificates or renewal certificates or for an order for
the board to issue a CTO (section 38 of the Act),
• to cancel a CTO (section 38(1.1) of the Act).
SUBSTITUTE DECISION-MAKER (SDM)
A person who makes treatment decisions on behalf of a person who is a formal patient
or is subject to a CTO, when they are a minor or are not mentally competent. Although
the term SDM is never used in the Act, it is used in practice. Section 28 of the Act
specifies who may be an SDM.
VOLUNTARY PATIENT
A “voluntary patient” in the mental health context usually refers to a patient who is
admitted to a facility of their own volition for the purpose of receiving mental health
diagnosis or treatment.
For the purpose of this guide, included in this category are patients who are admitted for
mental health diagnosis or treatment in a facility by way of the consent of an SDM (e.g.,
guardian). In other materials, these individuals are sometimes referred to as “informal
patients”. Regardless of their categorization, they are not detained under admission or
renewal certificates, and thus in this manual are treated as “voluntary”.
Classification: Protected A 133
APPENDIX II: List of Designated Facilities
List of Designated Facilities
15.2(1) The following places are designated as facilities for the purposes of
section 1(1)(d) of the Act:
(a) Alberta Hospital Edmonton;
(b) Centennial Centre for Mental Health and Brain Injury;
(c) Peter Lougheed Centre;
(d) Foothills Medical Centre;
(e) Misericordia Community Hospital;
(f) Royal Alexandra Hospital;
(g) University of Alberta Hospital;
(h) Grey Nuns Community Hospital;
(i) Chinook Regional Hospital;
(j) Medicine Hat Regional Hospital;
(k) Northern Lights Regional Health Centre;
(l) repealed;
(m) Rockyview General Hospital;
(n) Claresholm Centre for Mental Health and Addictions;
(o) Red Deer Regional Hospital Centre;
(p) Southern Alberta Forensic Psychiatry Centre;
(q) St. Therese - St. Paul Healthcare Centre;
(r) Villa Caritas;
(s) South Health Campus;
(t) Alberta Children’s Hospital;
(u) Stollery Children’s Hospital;
(v) Grande Prairie Regional Hospital.
Classification: Protected A 134
(2) The following places are designated as facilities for the purposes of section
1(1)(d) of the Act, only for the purposes of section 13 of the Act:
(a) Helen Hunley Forensic Pavilion at Alberta Hospital Edmonton;
(b) Southern Alberta Forensic Psychiatry Centre.
(3) The following places are designated as facilities for the purposes of section
1(1)(d) of the Act, except for the purposes of sections 4(1)(a), 9.6, 10, 12 and 24 of the
Act:
(a) Glenrose Rehabilitation Hospital;

Classification: Protected A 135
APPENDIX III: Mental Health Act Forms
Electronic versions of all the Mental Health Act forms are available on the Alberta
Health Services website at https://www.albertahealthservices.ca/info/page1256.aspx .
These forms can be a) completed on the computer and then printed and signed, or b)
printed then completed by hand and signed. They may not be altered in any way.
Form 1:
Admission Certificate (section 2 of the Act)
Form 2:
Renewal Certificate (section 8 of the Act)
Form 2.1:
Cancellation of Admission Certificate or Renewal Certificate (section
31(4) of the Act)
Form 3:
Order to Return a Formal Patient to a Facility (sections 20(4) or 21(1) of
the Act)
Form 4:
Certificate of Transfer into Alberta (section 24(1) of the Act)
Form 5:
Transfer of Formal Patient to a Jurisdiction Outside Alberta (section 25 of
the Act)
Form 6:
Memorandum of Transfer to Another Facility (section 22(1) of the Act)
Form 7:
Information (section 10 of the Act)
Form 8:
Warrant (section 10 of the Act)
Form 9:
Extension of Warrant (section 11 of the Act)
Form 10:
Statement of Peace Officer on Apprehension (section 12 of the Act)
Form 11:
Certificate of Incompetence to Make Treatment Decisions (section 27 of
the Act)
Form 12:
Application For Review Panel Hearing (sections 27(3), 29(2), 33, 38(1)
and 38(1.1) of the Act)
Form 13:
Notice of Hearing Before Review Panel (section 40 of the Act)
Form 14:
Decision of Review Panel Regarding Mental Incompetence to Make
Treatment Decisions (sections 27(3) and 41 of the Act)
Form 15:
Decision of Review Panel Regarding Treatment (sections 29(2) and 41
of the Act)
Form 16:
Decision of Review Panel Regarding Transfer Back to a Correctional
Facility (sections 33 and 41 of the Act)
Classification: Protected A 136
Form 17:
Decision of Review Panel Regarding Admission Certificates, Renewal
Certificates, or Community Treatment Orders (sections 38(1), 38(1.1)
and 41 of the Act)
Form 17.1
Decision of Review Panel Regarding Order for the Board to Issue a
Community Treatment Order (sections 38(1)(b) and 41 of the Act)
Form 18:
Decision of Review Panel Regarding Renewal Certificates and
Community Treatment Orders (Deemed Application) (sections 39 and 41
of the Act)
Form 19:
Issuance of Community Treatment Order (section 9.1 of the Act)
Form 20:
Renewal of Community Treatment Order (section 9.3 of the Act)
Form 21:
Amendments to Community Treatment Order (section 9.4 of the Act)
Form 22:
Community Treatment Order, Cancellation or Expiry (section 9.5 of the
Act)
Form 23:
Community Treatment Order, Apprehension Order (section 9.6 of the
Act)
Form 24:
Community Treatment Order, Examination on Apprehension (section 9.6
of the Act)
Form 25:
Community Treatment Order, Non-compliance Report (section 9.1(2)(f)
of the Act)
Classification: Protected A 137
APPENDIX IV: Investigations that may occur within
Designated Facilities
Note: the wording in this section has been taken from the following
organizations’ websites.
What does the Alberta Ombudsman do?
The Alberta Ombudsman responds to complaints of unfair treatment by provincial
government authorities, municipalities, the Patient Concerns Resolution Process of
Alberta Health Services, health professions and other designated professional
organizations.
The Alberta Ombudsman’s website is https://www.ombudsman.ab.ca/.
Protection for Persons in Care
Protection for Persons in Care requires the reporting of abuse of adult clients receiving
care in publicly funded facilities.
The Protection for Persons in Care website is https://www.alberta.ca/protection-for-
persons-in-care.aspx.
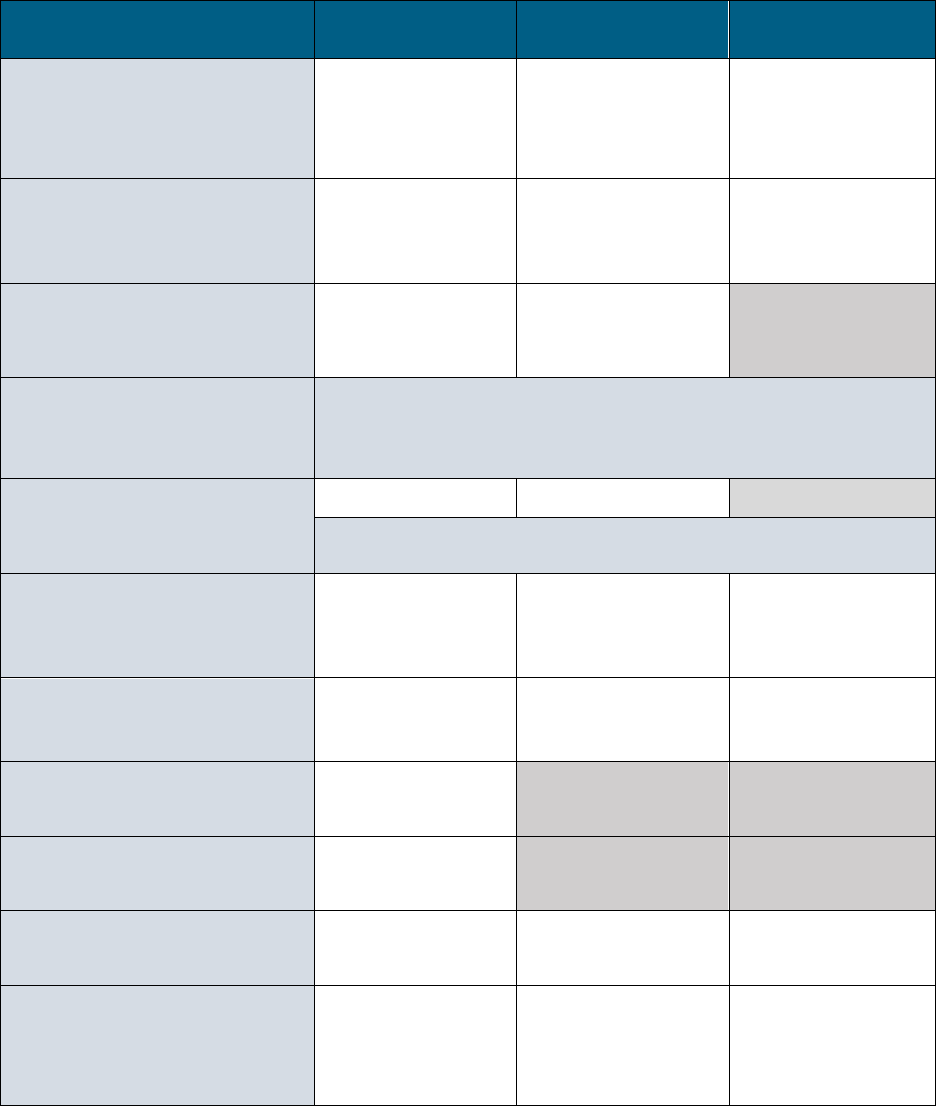
Classification: Protected A 138
APPENDIX V: Qualified Health Professionals Roles
under the Mental Health Act
MHA Forms completions by
Qualified Health Professionals
Psychiatrist Physician Nurse Practitioner
Form 1 - Issuance of Admission
Certificate
One of whom must be a
psychiatrist
Form 2 - Issuance of Renewal
Certificate
One of whom must be a
psychiatrist
Form 2.1 - Cancellation of
Admission or Renewal Certificate
Form 3 - Order to Return a Formal
Patient to a Facility
The responsibility of the “board” is delegated, and may be
delegated to any of these three groups
-
Form 11
Certificate of Incompetence to Make
Treatment Decisions
- If a formal patient who is competent or the substitute decision-maker object to
treatment, then the QHP shall not administer treatment without a treatment
order (issued by the review panel)
Form 19 & 20 - CTO Issuance &
Renewal
One of whom must be a
psychiatrist
Form 21 - CTO Amendment
One of whom must be a
psychiatrist
Form 22
CTO Cancellation
Form 22
CTO Expiry
Form 23
CTO Apprehension Order
Form 24
CTO Examination on Apprehension
One of whom must be a
psychiatrist
Classification: Protected A 139
Qualified Health Professional (QHP) as defined by the Act “qualified health professional” means a
psychiatrist, physician, nurse practitioner, or a person who is registered under section 33(1)(a) of the
Health Professions Act as a member of a health profession or of a category within a health profession
designated by the regulations for the purposes of all or part of the Act.
